Genetics of Endocrine and Neuroendocrine Neoplasias (PDQ®): Genetics - Health Professional Information [NCI]
Genetics of Endocrine and Neuroendocrine Neoplasias (PDQ®): Genetics - Health Professional Information [NCI]Skip to the navigationIntroductionMany of the medical and scientific terms used in this summary are found in the NCI Dictionary of Genetics Terms. When a linked term is clicked, the definition will appear in a separate window. Many of the genes described in this summary are found in the Online Mendelian Inheritance in Man (OMIM) database. When OMIM appears after a gene name or the name of a condition, click on OMIM for a link to more information. A concerted effort is being made within the genetics community to shift terminology used to describe genetic variation. The shift is to use the term "variant" rather than the term "mutation" to describe a difference that exists between the person or group being studied and the reference sequence. Variants can then be further classified as benign (harmless), likely benign, of uncertain significance, likely pathogenic, or pathogenic (disease causing). Throughout this summary, we will use the term pathogenic variant to describe a disease-causing mutation. Refer to the Cancer Genetics Overview summary for more information about variant classification. There are several hereditary syndromes that involve endocrine or neuroendocrine glands, such as multiple endocrine neoplasia type 1 (MEN1), multiple endocrine neoplasia type 2 (MEN2), pheochromocytoma (PHEO), paraganglioma (PGL), Li-Fraumeni syndrome, familial adenomatous polyposis, and von Hippel-Lindau syndrome. This summary currently focuses on MEN1, MEN2, familial PHEO and PGL syndrome, and Carney-Stratakis (CSS) syndrome. Li-Fraumeni syndrome, familial adenomatous polyposis, Cowden syndrome, and von Hippel-Lindau syndrome are discussed in the PDQ summaries on Genetics of Breast and Gynecologic Cancers; Genetics of Colorectal Cancer; and Genetics of Kidney Cancer. The term multiple endocrine neoplasia is used to describe a group of heritable tumors of endocrine tissues that may be benign or malignant. They are typically classified into two main categories: MEN1 (also known as Wermer syndrome) and MEN2. Historically, MEN2 has been further stratified into the following three subtypes based on the presence or absence of certain endocrine tumors in the individual or family: MEN2A, familial medullary thyroid carcinoma, and MEN2B. The tumors usually manifest themselves by overproduction of hormones, tumor growth, or both. (Refer to the MEN1 and MEN2 sections of this summary for more information.) PGLs and PHEOs are rare tumors arising from chromaffin cells, which have the ability to synthesize, store, and secrete catecholamines and neuropeptides. In 2004, the World Health Organization characterized PHEOs as adrenal gland tumors and PGLs as extra-adrenal tumors.[1] Either tumor may occur sporadically, as a manifestation of a hereditary syndrome, or as the sole tumor in familial PGL and PHEO syndrome. (Refer to the Familial PHEO and PGL Syndrome section of this summary for more information.) Affected individuals with CSS have multifocal, locally aggressive gastrointestinal stromal tumors and multiple neck, intrathoracic, and intra-abdominal PGLs at relatively early ages.[2,3,4] Although similarly named, this syndrome is distinct from Carney Complex and Carney Triad. (Refer to the CSS section of this summary for more information.) References:
-
DeLellis RA, Lloyd RV, Heitz PU, et al., eds.: Pathology and Genetics of Tumours of Endocrine Organs. Lyon, France: IARC Press, 2004. World Health Organization classification of tumours, vol. 8.
-
Carney JA, Stratakis CA: Familial paraganglioma and gastric stromal sarcoma: a new syndrome distinct from the Carney triad. Am J Med Genet 108 (2): 132-9, 2002.
-
McWhinney SR, Pasini B, Stratakis CA, et al.: Familial gastrointestinal stromal tumors and germ-line mutations. N Engl J Med 357 (10): 1054-6, 2007.
-
Pasini B, McWhinney SR, Bei T, et al.: Clinical and molecular genetics of patients with the Carney-Stratakis syndrome and germline mutations of the genes coding for the succinate dehydrogenase subunits SDHB, SDHC, and SDHD. Eur J Hum Genet 16 (1): 79-88, 2008.
Multiple Endocrine Neoplasia Type 1Clinical Description Multiple endocrine neoplasia type 1 (MEN1) (OMIM) is an autosomal dominant syndrome, with an estimated prevalence of about 1 in 30,000 individuals.[1] The major endocrine features of MEN1 include the following: - Parathyroid tumors and primary hyperparathyroidism (PHPT).
- Duodenopancreatic neuroendocrine tumors (NETs).
- Pituitary tumors.
A clinical diagnosis of MEN1 is made when an individual has two of these three major endocrine tumors. Familial MEN1 is defined as at least one MEN1 case plus at least one first-degree relative (FDR) with one of these three tumors, or two FDRs with a germline pathogenic variant.[2,3,4] Initial clinical presentation of symptoms typically occurs between the ages of 20 years and 30 years, although a diagnosis of MEN1 may not be confirmed for many more years. The age-related penetrance of MEN1 is 45% to 73% by age 30 years, 82% by age 50 years, and 96% by age 70 years.[2,5,6] Parathyroid Tumors and PHPT The most common features and often the first presenting signs of MEN1 are parathyroid tumors, which result in PHPT. These tumors occur in 80% to 100% of patients by age 50 years.[2,7,8,9] Unlike the solitary adenoma seen in sporadic cases, MEN1-associated parathyroid tumors are typically multiglandular and often hyperplastic.[10] The mean age at onset of PHPT in MEN1 is 20 to 25 years, in contrast to that in the general population, which is typically age 50 to 59 years. Parathyroid carcinoma in MEN1 is rare but has been described.[11,12,13,14] Individuals with MEN1-associated PHPT will have elevated parathyroid hormone (PTH) and calcium levels in the blood. The clinical manifestations of PHPT are mainly the result of hypercalcemia. Mild hypercalcemia may go undetected and have few or no symptoms. More severe hypercalcemia can result in the following: - Constipation.
- Nausea and vomiting.
- Dehydration.
- Decreased appetite and abdominal pain.
- Anorexia.
- Diuresis.
- Kidney stones.
- Increased bone resorption with resultant increased risk of bone fracture.
- Lethargy.
- Depression.
- Confusion.
- Hypertension.
- Shortened QT interval.
Since MEN1-associated hypercalcemia is directly related to the presence of parathyroid tumors, surgical removal of these tumors may result in normalization of calcium and PTH levels and relief of symptoms; however, high recurrence rates following surgery have been reported in some series.[15,16,17] (Refer to the Interventions section of this summary for more information.) Duodenopancreatic NETs Duodenopancreatic NETs are the second most common endocrine manifestation in MEN1, occurring in 30% to 80% of patients by age 40 years.[2,9] Duodenopancreatic NETs seen in MEN1 include the following: - Gastrinomas.
- Nonfunctioning NETs.
- Insulinomas.
- Vasoactive intestinal peptide tumors (VIPomas).
- Glucagonomas.
- Somatostatinomas.
Table 1. MEN1-Associated Duodenopancreatic Neuroendocrine Tumors| Tumor type | Estimated Penetrance | Symptoms |
|---|
| MEN1 = multiple endocrine neoplasia type 1. | | Gastrinoma | ≤70%[18,19] | Peptic ulcer disease and esophagitis | | Diarrhea | | Abdominal pain | | Weight loss | | Nonfunctioning | 20%-55%[18,20] | Local compressive symptoms: abdominal pain, jaundice, anorexia, weight loss | | Insulinoma | 10%[18] | Whipple's triad: symptomatic hypoglycemia reversed by glucose administration with associated elevation of insulin, C-peptide, and proinsulin levels | | Vasoactive intestinal peptide | 1%[18,21] | Watery diarrhea | | Hypokalemia | | Achlorhydria | | Glucagonoma | 1%[18,21] | Diabetes mellitus | | Diarrhea | | Depression | | Necrolytic migratory erythema | | Thromboembolic disease | | Somatostatinoma | <1%[21] | Diabetes mellitus | | Diarrhea/steatorrhea | | Gallbladder disease | | Hypochlorhydria | | Weight loss | Gastrinomas represent 50% of the gastrointestinal NETs in MEN1 and are the major cause of morbidity and mortality in MEN1 patients.[2,15] Gastrinomas are usually multicentric, with small (<0.5 cm) foci throughout the duodenum.[22] Most result in peptic ulcer disease (Zollinger-Ellison syndrome), and half are malignant at the time of diagnosis.[15,22,23] Nonfunctioning duodenopancreatic NETs were originally thought to be relatively uncommon tumors in individuals with MEN1. With the advent of genetic testing and improved imaging techniques, however, their prevalence in MEN1 has increased, with one study showing a frequency as high as 55% by age 39 years in carriers of MEN1pathogenic variants undergoing prospective endoscopic ultrasound of the pancreas.[20,24] These tumors can be metastatic. One study of 108 carriers of MEN1 pathogenic variants with nonfunctioning duodenopancreatic NETs showed a positive correlation between tumor size and rate of metastasis and death, with tumors larger than 2 cm having significantly higher rates of metastasis than those smaller than 2 cm.[25] (Refer to the Molecular Genetics of MEN1 section of this summary for more information about MEN1gene pathogenic variants.) Pituitary Tumors Approximately 15% to 50% of MEN1 patients will develop a pituitary tumor.[2,9] Two-thirds are microadenomas (<1.0 cm in diameter), and the majority are prolactin-secreting.[26] Other pituitary tumors can include somatotropinomas and corticotropinomas, or they may be nonfunctioning. Table 2. MEN1-Associated Pituitary Tumors| Tumor type | Estimated Penetrance | Symptoms |
|---|
| MEN1 = multiple endocrine neoplasia type 1. | | Prolactinoma | 20%[18] | Galactorrhea | | Amenorrhea/infertility | | Hypogonadism | | Somatotropinoma | 10%[18] | Coarse facial features | | Soft tissue overgrowth: enlargement of hands/feet | | Hyperhidrosis | | Corticotropinoma | <5%[18] | Weight gain | | Hypertension | | Flushing | | Easy bruising/bleeding | | Hyperglycemia | Other MEN1-Associated Tumors Other manifestations of MEN1 include carcinoids of the foregut (5%-10% of MEN1 patients). These are typically bronchial or thymic and are sometimes gastric. Skin lesions are also common and can include facial angiofibromas (up to 80% of MEN1 patients) and collagenomas (~75% of MEN1 patients).[27] Lipomas (~30% of MEN1 patients) and adrenal cortical lesions (up to 50% of MEN1 patients), including cortical adenomas, diffuse or nodular hyperplasia, or rarely, carcinoma are also common.[28,29,30] The following manifestations have also been reported:[31,32,33] - Thyroid adenomas.
- Pheochromocytoma.
- Spinal ependymoma.
- Meningioma.
- Leiomyoma (e.g., esophageal, lung, and uterine).
Making the Diagnosis of MEN1 MEN1 is often difficult to diagnose in the absence of a significant family history or a positive genetic test for a pathogenic variant in the MEN1 gene. One study of 560 individuals with MEN1 showed a significant delay between the time of the first presenting symptom and the diagnosis of MEN1.[34] This time lapse is likely because some presenting symptoms of MEN1-associated tumors, such as amenorrhea, peptic ulcers, hypoglycemia, and nephrolithiasis, are not specific to MEN1. Furthermore, identification of an MEN1-associated tumor is not sufficient to make the clinical diagnosis of MEN1 and may not trigger a referral to an endocrinologist. The median time between the first presenting symptom and diagnosis of MEN1 ranges from 7.6 years to 12 years.[5,29] Genetic testing alleviates some of this delay. Several studies have shown statistically significant differences in the age at MEN1 diagnosis between probands and their family members. In one study, clinically symptomatic probands were diagnosed with MEN1 at a mean age of 47.5 years (standard deviation [SD] +/- 13.5 years), while family members were diagnosed at a mean age of 38.5 years (SD +/- 15.4 years; P < .001).[34] In another study of 154 individuals with MEN1, probands were diagnosed at a mean age of 39.5 years (range: 18-74 years), compared with a mean age of 27 years (range: 14-56 years; P <.05) in family members diagnosed by predictive genetic testing.[35] Nonetheless, the lag time between the diagnosis of MEN1 in an index case and the diagnosis of MEN1 in family members can be significant, leading to increased morbidity and mortality.[36] This was demonstrated in a recent Dutch MEN1 Study Group analysis, which showed that 10% to 38% of non-index cases already had an MEN1-related manifestation at diagnosis; 4% of these individuals died of an MEN1-related cause that developed during or before the lag time. In family members, the majority of the morbidity related to lag time was due to metastatic duodenopancreatic NETs, pituitary macroadenomas, and multiple MEN1 manifestations.[36] These findings underscore the importance of increased awareness of the signs and symptoms of MEN1-related tumors and the constellation of findings necessary to suspect the diagnosis. It also highlights the importance of genetic counseling and testing and communication among family members once a diagnosis of MEN1 is made. Figure 1 illustrates some of the challenges in identifying MEN1 in a family. 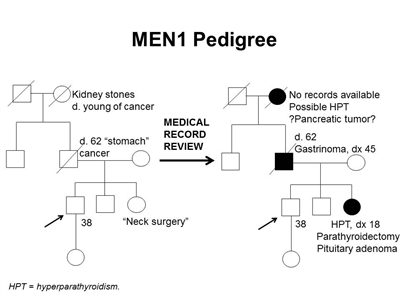
Figure 1. MEN1 pedigree. MEN1 can be very difficult to identify in a pedigree. The pedigree on the left was constructed based on self-report, and the pedigree on the right depicts the same family following a review of available medical records. This pedigree shows some of the features of a family with an MEN1 pathogenic variant across four generations, including affected family members with hyperparathyroidism, a pituitary adenoma, gastrinoma, and a suspected pancreatic tumor. The tumors in MEN1 typically occur at an earlier age than their sporadic counterparts. MEN1 families may exhibit some or all of these features. As an autosomal dominant syndrome, transmission can occur through maternal or paternal lineages, as depicted in the figure.
Since many of the tumors in MEN1 are underdiagnosed or misdiagnosed, identifying an MEN1 gene pathogenic variant in the proband early in the disease process can allow for early detection and treatment of tumors and earlier identification of at-risk family members. Many studies have been performed to determine the prevalence of MEN1 gene pathogenic variants among patients with apparently sporadic MEN1-related tumors. For example, approximately one-third of patients with Zollinger-Ellison syndrome will carry an MEN1 pathogenic variant.[37,38] In individuals with apparently isolated PHPT or pituitary adenomas, the pathogenic variant prevalence is lower, on the order of 2% to 5%,[26,39,40] but the prevalence is higher in individuals diagnosed with these tumors before age 30 years. Some authors suggest referral for genetics consultation and/or genetic testing for pathogenic variants in MEN1 if one of the following conditions is present:[18,41,42] - Gastrinoma at any age in the individual or an FDR.
- Multifocal duodenopancreatic NETs at any age.
- PHPT before age 30 or 40 years.
- Multiglandular parathyroid adenomas/hyperplasia or recurrent PHPT.
- Presence of one of the three main MEN1 tumors plus one of the less common tumors/findings.
- Presence of two or more features (e.g., adrenal adenomas and carcinoid tumor).
- Combination of at least two of the following in one individual: parathyroid adenoma; thymic, bronchial, or foregut carcinoid tumor; duodenopancreatic NET; pituitary tumor; adrenal tumor.
- Parathyroid adenoma and a family history of hyperparathyroidism, pituitary adenoma, duodenopancreatic NET, or foregut carcinoid tumor.
- Multiple primary duodenopancreatic NETs in the same person.
Molecular Genetics of MEN1 The MEN1 gene is located on chromosome 11q13 and encodes the protein menin.[3,43,44] Over 1,300 pathogenic variants have been identified in the MEN1 gene to date, and these are scattered across the entire coding region.[45] Most (~65%) of these are nonsense or frameshift variants. The remainder are missense variants (20%), which lead to expression of an altered protein, splice-site variants (9%), or partial- or whole-gene deletions (1%-4%). There is some evidence of genotype -phenotype correlations, but inter- and intra-familial variability is common.[46,47] One large study demonstrated the highest rates of heritability for pituitary, adrenal, and thymic NETs.[48] Genetic Testing and Differential Diagnosis Genetic testing for MEN1 pathogenic variants is recommended for individuals meeting clinical diagnostic criteria and may be considered in a subset of the less common tumors. (Refer to the bulleted list in the Making the diagnosis of MEN1 section of this summary for more information.) For individuals meeting diagnostic criteria, the pathogenic variant detection rate is approximately 75% to 90%.[46,49] Still, germline pathogenic variant yield ranged from 16% to 38% for apparently sporadic cases of parathyroid (15.8%), pancreatic islet (25.0%), or pituitary (37.5%) tumors, warranting consideration of genetic testing in these individuals because a diagnosis of MEN1 would prompt screening for other MEN1-related tumors.[50] Many commercial laboratories currently offering MEN1 testing use DNA sequencing as their primary method. Several offer additional analysis for partial- or whole-gene deletion and/or duplication, although such variants are rare and deletion/duplication testing is often reserved for individuals or families in which there is a very high clinical suspicion. Genetic testing for MEN1 pathogenic variants can be used to distinguish between MEN1 and other forms of hereditary hyperparathyroidism, such as familial isolated hyperparathyroidism (FIHP) (OMIM), hyperparathyroidism-jaw tumor syndrome (HPT-JT), and familial hypocalciuric hypercalcemia (FHH). The hyperparathyroidism in FHH is not primary hyperparathyroidism, which is seen in MEN1, HPT-JT and FIHP. HPT-JT, which is caused by germline pathogenic variants in the HRPT2 gene, is associated with PHPT, ossifying lesions of the maxilla and mandible, and renal lesions, usually bilateral renal cysts, hamartomas, and in some cases, Wilms tumor.[51,52] Unlike MEN1, HPT-JT is associated with an increased risk of parathyroid carcinoma.[53] FIHP, as its name suggests, is characterized by isolated PHPT with no additional endocrine features; in some families, FIHP is the initial diagnosis of what later develops into MEN1, HPT-JT, or FHH.[54,55,56] Approximately 20% of families with a clinical diagnosis of FIHP carry germline MEN1 pathogenic variants.[55,57,58] Pathogenic variants in the calcium-sensing receptor (CaSR) gene cause FHH, which can closely mimic the hyperparathyroidism in MEN1. Distinguishing between MEN1 and FHH can be critical in terms of management, as removal of the parathyroid glands in FHH does not correct the patient's hyperparathyroidism and results in unnecessary surgery without relief of symptoms.[59] Given the differential risks and management of these conditions and the increased risk of parathyroid carcinoma in HPT-JT, genetic diagnosis in a patient presenting with early-onset hyperparathyroidism may play an important role in the management of these patients and their families.[60] Refer to Table 3 for a summary of the clinical features of MEN1 and other forms of hereditary hyperparathyroidism. Table 3. Major Clinical Features of MEN1, FIHP, HPT-JT, and FHH| Condition | Gene(s) | Major Clinical Features |
|---|
| CaSR=calcium-sensing receptor gene; FHH = familial hypocalciuric hypercalcemia; FIHP = familial isolated hyperparathyroidism; HPT-JT = hyperparathyroidism-jaw tumor syndrome;HRPT2=hyperparathyroidism 2gene; MEN1 = multiple endocrine neoplasia type 1 (gene is italicized); NETs = neuroendocrine tumors; PHPT = primary hyperparathyroidism. | | MEN1 | MEN1 | PHPT, pituitary adenomas, duodenopancreatic NETs[10] | | FIHP | MEN1,HRPT2 | PHPT[54,55,56,57,58] | | HPT-JT | HRPT2 | PHPT; osteomas of maxilla and mandible; renal cysts or hamartomas; and rarely, Wilms tumor and parathyroid carcinoma[51,52,53] | | FHH | CaSR | Hyperparathyroidism (not primary)[59,61] | Surveillance Screening and surveillance for MEN1 may employ a combination of biochemical tests and imaging. Available recommendations are summarized in Table 4.[4,18] Table 4. Practice Guidelines for Surveillance of MEN1a| Biochemical Test or Procedure | Condition Screened For | Age Screening Initiated (y) | Frequency |
|---|
| CT = computed tomography; MEN1 = multiple endocrine neoplasia type 1; MRI = magnetic resonance imaging; NETs = neuroendocrine tumors; PHPT = primary hyperparathyroidism; PTH = parathyroid hormone. | | a Adapted from Brandi et al.[4]and Thakker et al.[18]. | | b The recommendations for abdominal imaging differ between two published guidelines for the diagnosis and management of MEN1.[4,18]There is weak evidence at this time to support annual imaging before age 10 years. Imaging before age 10 years does identify disease in a high proportion of patients, but it is not clear whether this impacts prognosis.[20,62] | | c The age to initiate screening and the screening frequency for pituitary tumors may be debatable because the clinical significance of small, nonfunctional tumors is unclear;[63]further study may be warranted. | | Serum prolactin and/or insulin-like growth factor 1 | Pituitary tumors | 5 | Every 1 y | | Fasting total serum calcium and/or ionized calcium and PTH | Parathyroid tumors and PHPT | 8 | Every 1 y | | Fasting serum gastrin | Duodenopancreatic gastrinoma | 20 | Every 1 y | | Chromogranin A, pancreatic polypeptide, glucagon, and vasointestinal polypeptide | Duodenopancreatic NETs | <10 | Every 1 y | | Fasting glucose and insulin | Insulinoma | 5 | Every 1 y | | Brain MRIc | Pituitary tumors | 5 | Every 3-5 y based on biochemical results | | Abdominal CT or MRIb[4] | Duodenopancreatic NETs | 20 | Every 3-5 y based on biochemical results | | Abdominal CT, MRI, or endoscopic ultrasoundb[18] | Duodenopancreatic NETs | <10 | Every 1 y | Interventions Surgical management of MEN1 is complex and controversial, given the multifocal and multiglandular nature of the disease and the high risk of tumor recurrence even after surgery. Establishing the diagnosis of MEN1 before making surgical decisions and referring affected individuals to a surgeon with experience in treating MEN1 can be critical in preventing unnecessary surgeries or inappropriate surgical approaches. Treatment for Parathyroid tumors Once evidence of parathyroid disease is established biochemically, the recommended course of action is surgical removal of the parathyroid glands. The timing and the extent of surgery, however, remain controversial.[64] Preoperative genetic testing helps guide the extent of surgery and can increase the likelihood of successful initial surgery and lower the likelihood of recurrent disease if a pathogenic variant is detected.[60] Some groups reserve surgical intervention for symptomatic patients, with continued annual biochemical screening for those who are asymptomatic. Once surgery is necessary, subtotal parathyroidectomy (removal of 3-3.5 glands) is often suggested as the initial treatment.[60] However, the rate of recurrence is quite high (55%-66%), and reoperation is often necessary.[15,16,17,60] Total parathyroidectomy with autotransplantation of parathyroid tissue to the forearm is also an option. A benefit of this approach is the easier removal of recurrent disease from the forearm than from the neck. Although the likelihood of recurrence is lowered by more extensive surgery, this must be weighed against the risk of rendering the patient hypoparathyroid.[65,66] Studies showing that concomitant bilateral cervical thymectomy decreases the rate of recurrence suggest that the thymus be removed at the initial operation.[65] If the devastating complication of hypocalcemia occurs, management requires oral calcitriol and calcium supplementation. This daily drug dependence can be a major burden on patients. Treatment for Duodenopancreatic NETs The timing and extent of surgery for duodenopancreatic NETs are controversial and depend on many factors, including severity of symptoms, extent of disease, functional component, location and necessity of simple enucleation, subtotal or total pancreatectomy, and pancreaticoduodenectomy (Whipple procedure). Specifically, tumor size has been suggested to advocate surgical resection based on the increased propensity for risk of metastases or recurrence with increased tumor diameter.[67] Unfortunately, there is no specific tumor marker or combination of tumor markers that are predictive of disease-specific mortality.[68] Long-acting somatostatin analogs may have a role in early-stage MEN1 duodenopancreatic NETs.[69] Initial study results of pharmacologic therapy suggest that the treatment is safe and that long-term suppression of tumor and hormonal activity can be seen in up to 10% of patients and stability of hormone hyperfunction in 80% of patients.[69] The primary goal of surgery is to improve long-term survival by reducing symptoms associated with hormone excess and lowering the risk of distant metastasis.[23] Surgery is commonly performed for most functional tumors and for nonfunctioning NETs when the tumor exceeds 2 to 3 cm because the likelihood of distant metastases is high.[70,71] Tumor size does seem to influence patient survival, with patients with smaller tumors having increased survival after resection.[72] While more-extensive surgical approaches (e.g., pancreatoduodenectomy) have been associated with higher cure rates and improved overall survival,[73,74,75] they also have higher rates of postoperative complications and long-term morbidity.[76] Therefore, the risks and benefits should be carefully considered, and surgical decisions should be made on a case-by-case basis. With regard to open or laparoscopic approaches, pancreatic laparoscopic surgery appears to be safe and associated with a shorter length of stay and fewer complications in selected patients.[77] Individuals with MEN1 who are diagnosed with NETs often have multiple tumors of various types throughout the pancreas and duodenum, some of which can be identified using magnetic resonance imaging or computed tomography. Many tumors, however, are too small to be detected using standard imaging techniques, and intra-arterial secretin stimulation testing and/or intraoperative ultrasound may be useful.[78,79] Preoperative assessment using various biochemical and imaging modalities, intraoperative assessment of tumor burden, and resolution of hormonal hyper-secretion are critical and, in some series, have been associated with higher cure rates and longer disease-free intervals.[78,79,80,81] In the current era of effective treatment for hyperfunctional hormone excess states, most MEN1-related deaths are due to the malignant nature of duodenopancreatic NETs. A less common but important risk of death is from malignant thymic carcinoid tumors. Indicators of a poor MEN1 prognosis include elevated fasting serum gastrin, the presence of functional hormonal syndromes, liver or distant metastases, aggressive duodenopancreatic NET growth, large duodenopancreatic NET size, or the need for multiple parathyroidectomies. The most common cause of non-MEN1-related death in this patient cohort is from cardiovascular disease.[82] Other duodenopancreatic NETs Glucagonomas, VIPomas, and somatostatinomas are rare but often have higher rates of malignancy than other duodenopancreatic NETs.[21] These are often treated with aggressive surgery.[83] Insulinomas Medical management of insulinoma using diet and medication is often unsuccessful; the mainstay of treatment for this tumor is surgery.[18] Insulinomas in MEN1 patients can be located throughout the pancreas, with a preponderance found in the distal gland,[84,85,86] and have a higher rate of metastasis than sporadic insulinoma.[83] Surgery can range from enucleation of single or multiple large tumors to partial pancreatic resection, or both,[85] to subtotal or total pancreatectomy.[84,85] More-extensive surgical approaches are associated with a lower rate of recurrence [73,74,85,87] but a higher rate of postoperative morbidity. Because insulinoma often occurs in conjunction with nonfunctioning pancreatic tumors, the selective intra-arterial calcium-injection test (SAS test) may be necessary to determine the source of insulin excess.[88] Intraoperative monitoring of insulin/glucose can help determine whether insulin-secreting tumors have been successfully excised.[79,89] Gastrinomas Most MEN1-associated gastrinomas originate in the duodenum. These tumors are typically multifocal and cause hyper-secretion of gastrin, with resultant peptic ulcer disease (Zollinger-Ellison syndrome). The multifocal nature makes complete surgical resection difficult. It is critical to manage symptoms before considering any type of surgical intervention. Historically, some groups have recommended close observation of individuals with smaller tumors (<2.0 cm on imaging) who have relief of symptoms using medications (e.g., proton pump inhibitors or histamine-2 agonists);[90] however, this approach may not be optimal for all patients. Several published series have shown a positive correlation between primary tumor size and rate of distant metastasis. One retrospective study showed that 61% of patients with tumors larger than 3 cm had liver metastases.[23] In another series, 40% of patients with tumors larger than 3 cm had liver metastases.[91] In contrast, both of these series showed significantly lower rates of liver metastases in individuals with tumors smaller than 3 cm (32% and 4.8%, respectively). On the basis of these and other data, many groups recommend surgery in individuals with nonmetastatic gastrinoma who have tumors larger than 2 cm.[18,75] The type of surgery for gastrinoma depends on many factors. A Whipple procedure is typically discouraged as an initial surgery, given the high postoperative morbidity and long-term complications, such as diabetes mellitus and malabsorption. Less extensive surgeries have been described with varying results. At a minimum, duodenectomy with intraoperative palpation and/or ultrasound to locate and excise duodenal tumors and peri-pancreatic lymph node dissection are performed.[78,92] Because most patients with gastrinoma will have concomitant NETs throughout the pancreas, some of which may be nonfunctional, some groups recommend resection of the distal pancreas and enucleation of tumors in the pancreatic head in addition to duodenal tumor excision.[78,92,93] Nonfunctioning NETs Approximately 50% of individuals with MEN1 will develop nonfunctioning NETs.[20,25] These are often identified incidentally during assessment and exploration for functioning tumors. As with gastrinomas, the metastatic rate is correlated with larger tumor size.[25] Tumors smaller than 1.5 cm are not likely to have lymph node metastases,[94] although the presence of metastatic disease has been associated with earlier age at death than in those without duodenopancreatic NETs.[25,95] Pituitary tumors Medical therapy to suppress hypersecretion is often the first line of therapy for MEN1-associated pituitary tumors. In one series of 136 patients, medical therapy was successful in approximately one-half of patients with secreting tumors (49 of 116, 42%), and successful suppression was correlated with smaller tumor size.[96] Surgery is often necessary for patients who are resistant to this treatment. Radiation therapy is reserved for patients with incomplete surgical resection.[18,97] References:
-
Agarwal SK, Ozawa A, Mateo CM, et al.: The MEN1 gene and pituitary tumours. Horm Res 71 (Suppl 2): 131-8, 2009.
-
Trump D, Farren B, Wooding C, et al.: Clinical studies of multiple endocrine neoplasia type 1 (MEN1) QJM 89 (9): 653-69, 1996.
-
Chandrasekharappa SC, Guru SC, Manickam P, et al.: Positional cloning of the gene for multiple endocrine neoplasia-type 1. Science 276 (5311): 404-7, 1997.
-
Brandi ML, Gagel RF, Angeli A, et al.: Guidelines for diagnosis and therapy of MEN type 1 and type 2. J Clin Endocrinol Metab 86 (12): 5658-71, 2001.
-
Carty SE, Helm AK, Amico JA, et al.: The variable penetrance and spectrum of manifestations of multiple endocrine neoplasia type 1. Surgery 124 (6): 1106-13; discussion 1113-4, 1998.
-
Goudet P, Dalac A, Le Bras M, et al.: MEN1 disease occurring before 21 years old: a 160-patient cohort study from the Groupe d'étude des Tumeurs Endocrines. J Clin Endocrinol Metab 100 (4): 1568-77, 2015.
-
Benson L, Ljunghall S, Akerström G, et al.: Hyperparathyroidism presenting as the first lesion in multiple endocrine neoplasia type 1. Am J Med 82 (4): 731-7, 1987.
-
Brandi ML, Marx SJ, Aurbach GD, et al.: Familial multiple endocrine neoplasia type I: a new look at pathophysiology. Endocr Rev 8 (4): 391-405, 1987.
-
Thakker RV: Multiple endocrine neoplasia type 1. In: DeGroot LJ, Besser M, Burger HG, eds.: Endocrinology. Volume 3. 3rd ed. Philadelphia, Pa: WB Saunders Co, 1995, pp 2815-31.
-
Chandrasekharappa SC, Teh BT: Clinical and molecular aspects of multiple endocrine neoplasia type 1. Front Horm Res 28: 50-80, 2001.
-
del Pozo C, García-Pascual L, Balsells M, et al.: Parathyroid carcinoma in multiple endocrine neoplasia type 1. Case report and review of the literature. Hormones (Athens) 10 (4): 326-31, 2011 Oct-Dec.
-
Agha A, Carpenter R, Bhattacharya S, et al.: Parathyroid carcinoma in multiple endocrine neoplasia type 1 (MEN1) syndrome: two case reports of an unrecognised entity. J Endocrinol Invest 30 (2): 145-9, 2007.
-
Shih RY, Fackler S, Maturo S, et al.: Parathyroid carcinoma in multiple endocrine neoplasia type 1 with a classic germline mutation. Endocr Pract 15 (6): 567-72, 2009 Sep-Oct.
-
Sato M, Miyauchi A, Namihira H, et al.: A newly recognized germline mutation of MEN1 gene identified in a patient with parathyroid adenoma and carcinoma. Endocrine 12 (3): 223-6, 2000.
-
Norton JA, Venzon DJ, Berna MJ, et al.: Prospective study of surgery for primary hyperparathyroidism (HPT) in multiple endocrine neoplasia-type 1 and Zollinger-Ellison syndrome: long-term outcome of a more virulent form of HPT. Ann Surg 247 (3): 501-10, 2008.
-
Hellman P, Skogseid B, Oberg K, et al.: Primary and reoperative parathyroid operations in hyperparathyroidism of multiple endocrine neoplasia type 1. Surgery 124 (6): 993-9, 1998.
-
Schreinemakers JM, Pieterman CR, Scholten A, et al.: The optimal surgical treatment for primary hyperparathyroidism in MEN1 patients: a systematic review. World J Surg 35 (9): 1993-2005, 2011.
-
Thakker RV, Newey PJ, Walls GV, et al.: Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J Clin Endocrinol Metab 97 (9): 2990-3011, 2012.
-
Norton JA, Krampitz G, Jensen RT: Multiple Endocrine Neoplasia: Genetics and Clinical Management. Surg Oncol Clin N Am 24 (4): 795-832, 2015.
-
Thomas-Marques L, Murat A, Delemer B, et al.: Prospective endoscopic ultrasonographic evaluation of the frequency of nonfunctioning pancreaticoduodenal endocrine tumors in patients with multiple endocrine neoplasia type 1. Am J Gastroenterol 101 (2): 266-73, 2006.
-
Lévy-Bohbot N, Merle C, Goudet P, et al.: Prevalence, characteristics and prognosis of MEN 1-associated glucagonomas, VIPomas, and somatostatinomas: study from the GTE (Groupe des Tumeurs Endocrines) registry. Gastroenterol Clin Biol 28 (11): 1075-81, 2004.
-
Pipeleers-Marichal M, Somers G, Willems G, et al.: Gastrinomas in the duodenums of patients with multiple endocrine neoplasia type 1 and the Zollinger-Ellison syndrome. N Engl J Med 322 (11): 723-7, 1990.
-
Weber HC, Venzon DJ, Lin JT, et al.: Determinants of metastatic rate and survival in patients with Zollinger-Ellison syndrome: a prospective long-term study. Gastroenterology 108 (6): 1637-49, 1995.
-
Tonelli F, Giudici F, Fratini G, et al.: Pancreatic endocrine tumors in multiple endocrine neoplasia type 1 syndrome: review of literature. Endocr Pract 17 (Suppl 3): 33-40, 2011 Jul-Aug.
-
Triponez F, Dosseh D, Goudet P, et al.: Epidemiology data on 108 MEN 1 patients from the GTE with isolated nonfunctioning tumors of the pancreas. Ann Surg 243 (2): 265-72, 2006.
-
Corbetta S, Pizzocaro A, Peracchi M, et al.: Multiple endocrine neoplasia type 1 in patients with recognized pituitary tumours of different types. Clin Endocrinol (Oxf) 47 (5): 507-12, 1997.
-
Darling TN, Skarulis MC, Steinberg SM, et al.: Multiple facial angiofibromas and collagenomas in patients with multiple endocrine neoplasia type 1. Arch Dermatol 133 (7): 853-7, 1997.
-
Machens A, Schaaf L, Karges W, et al.: Age-related penetrance of endocrine tumours in multiple endocrine neoplasia type 1 (MEN1): a multicentre study of 258 gene carriers. Clin Endocrinol (Oxf) 67 (4): 613-22, 2007.
-
Pieterman CR, Schreinemakers JM, Koppeschaar HP, et al.: Multiple endocrine neoplasia type 1 (MEN1): its manifestations and effect of genetic screening on clinical outcome. Clin Endocrinol (Oxf) 70 (4): 575-81, 2009.
-
Waldmann J, Bartsch DK, Kann PH, et al.: Adrenal involvement in multiple endocrine neoplasia type 1: results of 7 years prospective screening. Langenbecks Arch Surg 392 (4): 437-43, 2007.
-
Gibril F, Schumann M, Pace A, et al.: Multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome: a prospective study of 107 cases and comparison with 1009 cases from the literature. Medicine (Baltimore) 83 (1): 43-83, 2004.
-
McKeeby JL, Li X, Zhuang Z, et al.: Multiple leiomyomas of the esophagus, lung, and uterus in multiple endocrine neoplasia type 1. Am J Pathol 159 (3): 1121-7, 2001.
-
Vortmeyer AO, Lubensky IA, Skarulis M, et al.: Multiple endocrine neoplasia type 1: atypical presentation, clinical course, and genetic analysis of multiple tumors. Mod Pathol 12 (9): 919-24, 1999.
-
Yamazaki M, Suzuki S, Kosugi S, et al.: Delay in the diagnosis of multiple endocrine neoplasia type 1: typical symptoms are frequently overlooked. Endocr J 59 (9): 797-807, 2012.
-
Lourenço DM Jr, Toledo RA, Coutinho FL, et al.: The impact of clinical and genetic screenings on the management of the multiple endocrine neoplasia type 1. Clinics (Sao Paulo) 62 (4): 465-76, 2007.
-
van Leeuwaarde RS, van Nesselrooij BP, Hermus AR, et al.: Impact of Delay in Diagnosis in Outcomes in MEN1: Results From the Dutch MEN1 Study Group. J Clin Endocrinol Metab 101 (3): 1159-65, 2016.
-
Roy PK, Venzon DJ, Shojamanesh H, et al.: Zollinger-Ellison syndrome. Clinical presentation in 261 patients. Medicine (Baltimore) 79 (6): 379-411, 2000.
-
Bardram L, Stage JG: Frequency of endocrine disorders in patients with the Zollinger-Ellison syndrome. Scand J Gastroenterol 20 (2): 233-8, 1985.
-
Uchino S, Noguchi S, Sato M, et al.: Screening of the Men1 gene and discovery of germ-line and somatic mutations in apparently sporadic parathyroid tumors. Cancer Res 60 (19): 5553-7, 2000.
-
Scheithauer BW, Laws ER Jr, Kovacs K, et al.: Pituitary adenomas of the multiple endocrine neoplasia type I syndrome. Semin Diagn Pathol 4 (3): 205-11, 1987.
-
Newey PJ, Thakker RV: Role of multiple endocrine neoplasia type 1 mutational analysis in clinical practice. Endocr Pract 17 (Suppl 3): 8-17, 2011 Jul-Aug.
-
Hampel H, Bennett RL, Buchanan A, et al.: A practice guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: referral indications for cancer predisposition assessment. Genet Med 17 (1): 70-87, 2015.
-
Larsson C, Skogseid B, Oberg K, et al.: Multiple endocrine neoplasia type 1 gene maps to chromosome 11 and is lost in insulinoma. Nature 332 (6159): 85-7, 1988.
-
Bassett JH, Forbes SA, Pannett AA, et al.: Characterization of mutations in patients with multiple endocrine neoplasia type 1. Am J Hum Genet 62 (2): 232-44, 1998.
-
Lemos MC, Thakker RV: Multiple endocrine neoplasia type 1 (MEN1): analysis of 1336 mutations reported in the first decade following identification of the gene. Hum Mutat 29 (1): 22-32, 2008.
-
Giraud S, Zhang CX, Serova-Sinilnikova O, et al.: Germ-line mutation analysis in patients with multiple endocrine neoplasia type 1 and related disorders. Am J Hum Genet 63 (2): 455-67, 1998.
-
Wautot V, Vercherat C, Lespinasse J, et al.: Germline mutation profile of MEN1 in multiple endocrine neoplasia type 1: search for correlation between phenotype and the functional domains of the MEN1 protein. Hum Mutat 20 (1): 35-47, 2002.
-
Thevenon J, Bourredjem A, Faivre L, et al.: Unraveling the intrafamilial correlations and heritability of tumor types in MEN1: a Groupe d'étude des Tumeurs Endocrines study. Eur J Endocrinol 173 (6): 819-26, 2015.
-
Agarwal SK, Kester MB, Debelenko LV, et al.: Germline mutations of the MEN1 gene in familial multiple endocrine neoplasia type 1 and related states. Hum Mol Genet 6 (7): 1169-75, 1997.
-
Klein RD, Salih S, Bessoni J, et al.: Clinical testing for multiple endocrine neoplasia type 1 in a DNA diagnostic laboratory. Genet Med 7 (2): 131-8, 2005.
-
Teh BT, Farnebo F, Kristoffersson U, et al.: Autosomal dominant primary hyperparathyroidism and jaw tumor syndrome associated with renal hamartomas and cystic kidney disease: linkage to 1q21-q32 and loss of the wild type allele in renal hamartomas. J Clin Endocrinol Metab 81 (12): 4204-11, 1996.
-
Carpten JD, Robbins CM, Villablanca A, et al.: HRPT2, encoding parafibromin, is mutated in hyperparathyroidism-jaw tumor syndrome. Nat Genet 32 (4): 676-80, 2002.
-
Marx SJ: Multiple endocrine neoplasia type 1. In: Vogelstein B, Kinzler KW, eds.: The Genetic Basis of Human Cancer. New York, NY: McGraw-Hill, 1998, pp 489-506.
-
Warner J, Epstein M, Sweet A, et al.: Genetic testing in familial isolated hyperparathyroidism: unexpected results and their implications. J Med Genet 41 (3): 155-60, 2004.
-
Mizusawa N, Uchino S, Iwata T, et al.: Genetic analyses in patients with familial isolated hyperparathyroidism and hyperparathyroidism-jaw tumour syndrome. Clin Endocrinol (Oxf) 65 (1): 9-16, 2006.
-
Cetani F, Pardi E, Borsari S, et al.: Molecular pathogenesis of primary hyperparathyroidism. J Endocrinol Invest 34 (7 Suppl): 35-9, 2011.
-
Miedlich S, Lohmann T, Schneyer U, et al.: Familial isolated primary hyperparathyroidism--a multiple endocrine neoplasia type 1 variant? Eur J Endocrinol 145 (2): 155-60, 2001.
-
Cetani F, Pardi E, Ambrogini E, et al.: Genetic analyses in familial isolated hyperparathyroidism: implication for clinical assessment and surgical management. Clin Endocrinol (Oxf) 64 (2): 146-52, 2006.
-
Raue F, Frank-Raue K: Primary hyperparathyroidism--what the nephrologist should know--an update. Nephrol Dial Transplant 22 (3): 696-9, 2007.
-
Romero Arenas MA, Morris LF, Rich TA, et al.: Preoperative multiple endocrine neoplasia type 1 diagnosis improves the surgical outcomes of pediatric patients with primary hyperparathyroidism. J Pediatr Surg 49 (4): 546-50, 2014.
-
Christensen SE, Nissen PH, Vestergaard P, et al.: Familial hypocalciuric hypercalcaemia: a review. Curr Opin Endocrinol Diabetes Obes 18 (6): 359-70, 2011.
-
Langer P, Kann PH, Fendrich V, et al.: Prospective evaluation of imaging procedures for the detection of pancreaticoduodenal endocrine tumors in patients with multiple endocrine neoplasia type 1. World J Surg 28 (12): 1317-22, 2004.
-
de Laat JM, Dekkers OM, Pieterman CR, et al.: Long-Term Natural Course of Pituitary Tumors in Patients With MEN1: Results From the DutchMEN1 Study Group (DMSG). J Clin Endocrinol Metab 100 (9): 3288-96, 2015.
-
Hubbard JG, Sebag F, Maweja S, et al.: Primary hyperparathyroidism in MEN 1--how radical should surgery be? Langenbecks Arch Surg 386 (8): 553-7, 2002.
-
Pieterman CR, van Hulsteijn LT, den Heijer M, et al.: Primary hyperparathyroidism in MEN1 patients: a cohort study with longterm follow-up on preferred surgical procedure and the relation with genotype. Ann Surg 255 (6): 1171-8, 2012.
-
Lairmore TC, Govednik CM, Quinn CE, et al.: A randomized, prospective trial of operative treatments for hyperparathyroidism in patients with multiple endocrine neoplasia type 1. Surgery 156 (6): 1326-34; discussion 1334-5, 2014.
-
Kishi Y, Shimada K, Nara S, et al.: Basing treatment strategy for non-functional pancreatic neuroendocrine tumors on tumor size. Ann Surg Oncol 21 (9): 2882-8, 2014.
-
Qiu W, Christakis I, Silva A, et al.: Utility of chromogranin A, pancreatic polypeptide, glucagon and gastrin in the diagnosis and follow-up of pancreatic neuroendocrine tumours in multiple endocrine neoplasia type 1 patients. Clin Endocrinol (Oxf) 85 (3): 400-7, 2016.
-
Ramundo V, Del Prete M, Marotta V, et al.: Impact of long-acting octreotide in patients with early-stage MEN1-related duodeno-pancreatic neuroendocrine tumours. Clin Endocrinol (Oxf) 80 (6): 850-5, 2014.
-
Triponez F, Goudet P, Dosseh D, et al.: Is surgery beneficial for MEN1 patients with small (< or = 2 cm), nonfunctioning pancreaticoduodenal endocrine tumor? An analysis of 65 patients from the GTE. World J Surg 30 (5): 654-62; discussion 663-4, 2006.
-
Bettini R, Partelli S, Boninsegna L, et al.: Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery 150 (1): 75-82, 2011.
-
Brunner SM, Weber F, Werner JM, et al.: Neuroendocrine tumors of the pancreas: a retrospective single-center analysis using the ENETS TNM-classification and immunohistochemical markers for risk stratification. BMC Surg 15: 49, 2015.
-
Bartsch DK, Langer P, Wild A, et al.: Pancreaticoduodenal endocrine tumors in multiple endocrine neoplasia type 1: surgery or surveillance? Surgery 128 (6): 958-66, 2000.
-
Bartsch DK, Fendrich V, Langer P, et al.: Outcome of duodenopancreatic resections in patients with multiple endocrine neoplasia type 1. Ann Surg 242 (6): 757-64, discussion 764-6, 2005.
-
Norton JA, Jensen RT: Role of surgery in Zollinger-Ellison syndrome. J Am Coll Surg 205 (4 Suppl): S34-7, 2007.
-
Lopez CL, Waldmann J, Fendrich V, et al.: Long-term results of surgery for pancreatic neuroendocrine neoplasms in patients with MEN1. Langenbecks Arch Surg 396 (8): 1187-96, 2011.
-
Drymousis P, Raptis DA, Spalding D, et al.: Laparoscopic versus open pancreas resection for pancreatic neuroendocrine tumours: a systematic review and meta-analysis. HPB (Oxford) 16 (5): 397-406, 2014.
-
Imamura M, Komoto I, Ota S, et al.: Biochemically curative surgery for gastrinoma in multiple endocrine neoplasia type 1 patients. World J Gastroenterol 17 (10): 1343-53, 2011.
-
Tonelli F, Fratini G, Nesi G, et al.: Pancreatectomy in multiple endocrine neoplasia type 1-related gastrinomas and pancreatic endocrine neoplasias. Ann Surg 244 (1): 61-70, 2006.
-
Lewis MA, Thompson GB, Young WF Jr: Preoperative assessment of the pancreas in multiple endocrine neoplasia type 1. World J Surg 36 (6): 1375-81, 2012.
-
van Asselt SJ, Brouwers AH, van Dullemen HM, et al.: EUS is superior for detection of pancreatic lesions compared with standard imaging in patients with multiple endocrine neoplasia type 1. Gastrointest Endosc 81 (1): 159-167.e2, 2015.
-
Ito T, Igarashi H, Uehara H, et al.: Causes of death and prognostic factors in multiple endocrine neoplasia type 1: a prospective study: comparison of 106 MEN1/Zollinger-Ellison syndrome patients with 1613 literature MEN1 patients with or without pancreatic endocrine tumors. Medicine (Baltimore) 92 (3): 135-81, 2013.
-
Akerström G, Stålberg P: Surgical management of MEN-1 and -2: state of the art. Surg Clin North Am 89 (5): 1047-68, 2009.
-
O'Riordain DS, O'Brien T, van Heerden JA, et al.: Surgical management of insulinoma associated with multiple endocrine neoplasia type I. World J Surg 18 (4): 488-93; discussion 493-4, 1994 Jul-Aug.
-
Crippa S, Zerbi A, Boninsegna L, et al.: Surgical management of insulinomas: short- and long-term outcomes after enucleations and pancreatic resections. Arch Surg 147 (3): 261-6, 2012.
-
Sakurai A, Yamazaki M, Suzuki S, et al.: Clinical features of insulinoma in patients with multiple endocrine neoplasia type 1: analysis of the database of the MEN Consortium of Japan. Endocr J 59 (10): 859-66, 2012.
-
Vezzosi D, Cardot-Bauters C, Bouscaren N, et al.: Long-term results of the surgical management of insulinoma patients with MEN1: a Groupe d'étude des Tumeurs Endocrines (GTE) retrospective study. Eur J Endocrinol 172 (3): 309-19, 2015.
-
Grant CS: Insulinoma. Best Pract Res Clin Gastroenterol 19 (5): 783-98, 2005.
-
Giudici F, Nesi G, Brandi ML, et al.: Surgical management of insulinomas in multiple endocrine neoplasia type 1. Pancreas 41 (4): 547-53, 2012.
-
Mignon M, Cadiot G: Diagnostic and therapeutic criteria in patients with Zollinger-Ellison syndrome and multiple endocrine neoplasia type 1. J Intern Med 243 (6): 489-94, 1998.
-
Cadiot G, Vuagnat A, Doukhan I, et al.: Prognostic factors in patients with Zollinger-Ellison syndrome and multiple endocrine neoplasia type 1. Groupe d'Etude des Néoplasies Endocriniennes Multiples (GENEM and groupe de Recherche et d'Etude du Syndrome de Zollinger-Ellison (GRESZE). Gastroenterology 116 (2): 286-93, 1999.
-
Dickson PV, Rich TA, Xing Y, et al.: Achieving eugastrinemia in MEN1 patients: both duodenal inspection and formal lymph node dissection are important. Surgery 150 (6): 1143-52, 2011.
-
Akerström G, Stålberg P, Hellman P: Surgical management of pancreatico-duodenal tumors in multiple endocrine neoplasia syndrome type 1. Clinics (Sao Paulo) 67 (Suppl 1): 173-8, 2012.
-
Zhang IY, Zhao J, Fernandez-Del Castillo C, et al.: Operative Versus Nonoperative Management of Nonfunctioning Pancreatic Neuroendocrine Tumors. J Gastrointest Surg 20 (2): 277-83, 2016.
-
Goudet P, Murat A, Binquet C, et al.: Risk factors and causes of death in MEN1 disease. A GTE (Groupe d'Etude des Tumeurs Endocrines) cohort study among 758 patients. World J Surg 34 (2): 249-55, 2010.
-
Vergès B, Boureille F, Goudet P, et al.: Pituitary disease in MEN type 1 (MEN1): data from the France-Belgium MEN1 multicenter study. J Clin Endocrinol Metab 87 (2): 457-65, 2002.
-
Pieterman CR, Vriens MR, Dreijerink KM, et al.: Care for patients with multiple endocrine neoplasia type 1: the current evidence base. Fam Cancer 10 (1): 157-71, 2011.
Multiple Endocrine Neoplasia Type 2Clinical Description The endocrine disorders observed in multiple endocrine neoplasia type 2 (MEN2) are medullary thyroid cancer (MTC); its precursor, C-cell hyperplasia (CCH) (referred to as C-cell neoplasia or C-cell carcinoma in situ in more recent publications)[1]; pheochromocytoma (PHEO); and parathyroid adenomas and/or hyperplasia. MEN2-associated MTC is often bilateral and/or multifocal and arises in the background of CCH clonal C-cell proliferation. In contrast, sporadic MTC is typically unilateral and/or unifocal. Because approximately 75% to 80% of sporadic cases also have associated CCH, this histopathologic feature cannot be used as a predictor of familial disease.[2] Metastatic spread of MTC to regional lymph nodes (i.e., parathyroid, paratracheal, jugular chain, and upper mediastinum) or to distant sites, such as the liver, is common in patients who present with a palpable thyroid mass or diarrhea.[3,4] Although less than 1% of PHEOs metastasize, they can be clinically significant in cases of intractable hypertension or anesthesia-induced hypertensive crises. Parathyroid abnormalities in MEN2 can range from benign parathyroid adenomas or multigland hyperplasia to clinically evident hyperparathyroidism with hypercalcemia and renal stones. Historically, individuals and families with MEN2 were classified into one of the following three clinical subtypes based on the presence or absence of certain endocrine tumors in the individual or family: - MEN2A (OMIM).
- Familial medullary thyroid carcinoma (FMTC) (OMIM).
- MEN2B (OMIM).
Current stratification is moving away from a solely phenotype -based classification and more toward one that is based on genotype (i.e., the pathogenic variant) and phenotype.[5] Current recommendations propose two MEN2 syndromes: MEN2A and MEN2B. The MEN2A syndrome is further classified on the basis of the presence of associated conditions. For example, classical MEN2A includes those with MTC, PHEO, and/or hyperparathyroidism. Additional categories include MEN2A with cutaneous lichen amyloidosis (CLA), MEN2A with Hirschsprung disease (HSCR), and FMTC (presence of a RETgermline pathogenic variant and MTC but no family history of PHEO or hyperparathyroidism).[1] Classifying a patient or family by MEN2 subtype is useful in determining prognosis and management. The prevalence of MEN2 has been estimated to be approximately 1 in 35,000 individuals.[6] The vast majority of MEN2 cases are MEN2A. MTC and CCH MTC originates in calcitonin-producing cells (C-cells) of the thyroid gland. MTC is diagnosed when nests of C-cells extend beyond the basement membrane and infiltrate and destroy thyroid follicles. CCH is a controversial diagnosis, but most pathologists agree that it is defined as more than seven C-cells per cluster, complete follicles surrounded by C-cells, and C-cells in a distribution beyond normal anatomical location.[1,7,8,9] Individuals with RET (REarranged during Transfection) pathogenic variants and CCH are at substantially increased risk of progressing to MTC, although such progression is not universal.[10,11] MTC and CCH are suspected in the presence of an elevated plasma calcitonin concentration. A study of 10,864 patients with nodular thyroid disease found 44 (1 of every 250) cases of MTC after stimulation with calcitonin, none of which were clinically suspected. Consequently, half of these patients had no evidence of MTC on fine-needle biopsy and thus might not have undergone surgery without the positive calcitonin stimulation test.[12] CCH associated with a positive calcitonin stimulation test occurs in about 5% of the general population; therefore, the plasma calcitonin responses to stimulation do not always distinguish CCH from small MTC and cannot always distinguish between carriers and noncarriers in an MEN2 family.[10,11,13] MTC accounts for 2% to 3% of new cases of thyroid cancer diagnosed annually in the United States,[14] although this figure may be an underrepresentation of true incidence because of changes in diagnostic techniques. The total number of new cases of MTC diagnosed annually in the United States is between 1,000 and 1,200, about 75% of which are sporadic (i.e., they occur in the absence of a family history of either MTC or other endocrine abnormalities seen in MEN2). The peak incidence of the sporadic form is in the fifth and sixth decades of life.[3,15] A study in the United Kingdom estimated the incidence of MTC at 20 to 25 new cases per year among a population of 55 million.[16] In the absence of a positive family history, MEN2 may be suspected when MTC occurs at an early age or is bilateral or multifocal. While small series of apparently sporadic MTC cases have suggested a higher prevalence of germline RET pathogenic variants,[17,18] larger series indicate a prevalence range of 1% to 7%.[19,20] On the basis of these data, testing for pathogenic variants in the RETgene is widely recommended for all cases of MTC.[1,21,22,23] Level of evidence (Screening): 3 Natural history of MTC Thyroid cancer represents approximately 3% of new malignancies occurring annually in the United States, with an estimated 56,870 cancer diagnoses and 2,010 cancer deaths per year.[24] Of these cancer diagnoses, 2% to 3% are MTC.[14,25] MTC arises from the parafollicular calcitonin-secreting cells of the thyroid gland. MTC occurs in sporadic and familial forms and may be preceded by CCH, although CCH is a relatively common abnormality in middle-aged adults.[7,8] Average survival for MTC is lower than that for more common thyroid cancers (e.g., 83% 5-year survival for MTC compared with 90% to 94% 5-year survival for papillary and follicular thyroid cancer).[25,26] Survival is correlated with stage at diagnosis, and decreased survival in MTC can be accounted for in part by a high proportion of late-stage diagnosis.[25,26,27] In addition to early stage at diagnosis, other factors associated with improved survival in MTC include smaller tumor size, younger age at diagnosis, and diagnosis by biochemical screening (i.e., screening for calcitonin elevation) versus symptoms.[27,28,29,30] A Surveillance, Epidemiology, and End Results population-based study of 1,252 MTC patients found that survival varied by extent of local disease. For example, the 10-year survival rates ranged from 95.6% for those with disease confined to the thyroid gland to 40% for those with distant metastases.[28] Hereditary MTC While most MTC cases are sporadic, approximately 20% to 25% are hereditary because of pathogenic variants in the RET proto-oncogene.[31,32,33] Pathogenic variants in the RET gene cause MEN2, an autosomal dominant disorder associated with a high lifetime risk of MTC. Multiple endocrine neoplasia type 1 (MEN1) (OMIM) is an autosomal dominant endocrinopathy that is genetically and clinically distinct from MEN2; however, the similar nomenclature for MEN1 and MEN2 may cause confusion. There is no increased risk of thyroid cancer for MEN1. (Refer to the MEN1 section of this summary for more information.) MEN2-Related PHEO PHEOs (OMIM) arise from the catecholamine-producing chromaffin cells of the adrenal medulla. They are a relatively rare tumor and are suspected among patients with refractory hypertension or when biochemical screening reveals elevated excretion of catecholamines and catecholamine metabolites (i.e., norepinephrine, epinephrine, metanephrine, and vanillylmandelic acid) in 24-hour urine collections or plasma. In the past, measurement of urinary catecholamines was considered the preferred biochemical screening method. However, given that catecholamines are only released intermittently and are metabolized in the adrenal medulla into metanephrine and normetanephrine, the measurement of urine or plasma fractionated metanephrines has become the gold standard.[34,35,36,37,38,39] When biochemical screening in an individual who has or is at risk of MEN2 suggests PHEO, localization studies, such as magnetic resonance imaging (MRI) or computed tomography, can be performed.[40] Confirmation of the diagnosis can be made using iodine I 131-metaiodobenzylguanidine scintigraphy or positron emission tomography imaging.[11,40,41,42] A diagnosis of MEN2 is often considered in individuals with bilateral PHEO, those with an early age of onset (age <35 years), and those with a personal and/or family history of MTC or hyperparathyroidism. However, MEN2 is not the only genetic disorder that includes a predisposition to PHEO. Other disorders include neurofibromatosis type 1 (NF1), von Hippel-Lindau disease (VHL),[43] and the hereditary paraganglioma syndromes.[44] (Refer to the von Hippel-Lindau Syndrome section in the PDQ summary on the Genetics of Kidney Cancer for more information about VHL.) A large European consortium that included 271 patients from Germany,[45] 314 patients from France,[46] and 57 patients from Italy (total = 642) with apparently sporadic PHEO analyzed the known PHEO/functional paraganglioma susceptibility genes (NF1, RET, VHL, SDHB, and SDHD).[47] The diagnosis of NF1 in this series was made clinically, while all other conditions were diagnosed on the basis of the presence of a germline pathogenic variant in the causative gene. The disease was associated with a positive family history in 166 (25.9%) patients; germline pathogenic variants were detected in RET (n = 31), VHL (n = 56), NF1 (n = 14), SDHB (n = 34), or SDHD (n = 31). Rigorous clinical evaluation and pedigree analysis either before or after testing revealed that of those with a positive family history and/or a syndromic presentation, 58.4% carried a pathogenic variant, compared with 12.7% who were nonsyndromic and/or had no family history. Of the 31 individuals with a germline RET pathogenic variant, 28 (90.3%) had a positive family history and/or syndromic presentation, suggesting that most individuals with RET pathogenic variants and PHEO will have a positive family history or other manifestations of the disease. Primary Hyperparathyroidism (PHPT) PHPT is the third most common endocrine disorder in the general population. The incidence increases with age with the vast majority of cases occurring after the sixth decade of life. Approximately 80% of cases are the result of a single adenoma.[48] PHPT can also be seen as a component tumor in several different hereditary syndromes, including the following: - MEN1.
- Hyperparathyroidism-jaw tumor syndrome.
- Familial isolated hyperparathyroidism.
- MEN2.[49,50,51]
Hereditary PHPT is typically multiglandular, presents earlier in life, and can have histologic evidence of both adenoma and glandular hyperplasia. Clinical Diagnosis of MEN2 Subtypes The diagnosis of the two MEN2 clinical subtypes relies on a combination of clinical findings, family history, and molecular genetic testing of the RET gene (chromosomal region 10q11.2). MEN2A Classical MEN2A MEN2A is diagnosed clinically by the occurrence of two specific endocrine tumors in addition to MTC: PHEO and/or parathyroid adenoma and/or hyperplasia in a single individual or in close relatives.[1] The classical MEN2A subtype makes up about 60% to 90% of MEN2 cases. The MEN2A subtype was initially called Sipple syndrome.[52] Since genetic testing for RET pathogenic variants has become available, it has become apparent that about 95% of individuals with MEN2A will develop MTC.[11,53,54,55] MTC is generally the first manifestation of MEN2A. In asymptomatic at-risk individuals, stimulation testing may reveal elevated plasma calcitonin levels and the presence of CCH or MTC.[11,54] In families with MEN2A, the biochemical manifestations of MTC generally appear between the ages of 5 years and 25 years (mean, 15 years).[11] If presymptomatic screening is not performed, MTC typically presents as a neck mass or neck pain between the ages of about age 5 years and 20 years. More than 50% of such patients have cervical lymph node metastases.[3] Diarrhea, the most frequent systemic symptom, occurs in patients with a markedly elevated plasma calcitonin level or bulky disease and/or hepatic metastases and implies a poor prognosis.[1,3,56,57] Up to 30% of patients with MTC present with diarrhea and advanced disease.[58] MEN2-associated PHEOs are more often bilateral, multifocal, and associated with extratumoral medullary hyperplasia.[59,60,61] They also have an earlier age of onset and are less likely to be malignant than their sporadic counterparts.[59,62] MEN2-associated PHEOs usually present after MTC, typically with intractable hypertension.[63] Unlike the PHPT seen in MEN1, hyperparathyroidism in individuals with MEN2 is typically asymptomatic or associated with only mild elevations in calcium.[58,64] A series of 56 patients with MEN2-related hyperparathyroidism has been reported by the French Calcitonin Tumors Study Group.[64] The median age at diagnosis was 38 years, documenting that this disorder is rarely the first manifestation of MEN2. This is in sharp contrast to MEN1, in which the vast majority of patients (87%-99%) initially present with primary hyperparathyroidism.[65,66,67] Parathyroid abnormalities were found concomitantly with surgery for medullary thyroid carcinoma in 43 patients (77%). Two-thirds of the patients were asymptomatic. Among the 53 parathyroid glands removed surgically, there were 24 single adenomas, 4 double adenomas, and 25 hyperplastic glands. MEN2A with cutaneous lichen amyloidosis A small number of families with MEN2A have pruritic skin lesions known as cutaneous lichen amyloidosis. This lichenoid skin lesion is located over the upper portion of the back and may appear before the onset of MTC.[68,69] MEN2A with Hirschsprung disease (HSCR) HSCR (OMIM), a disorder of the enteric plexus of the colon that typically results in enlargement of the bowel and constipation or obstipation in neonates, is observed in a small number of individuals with RET pathologic variants.[70] Up to 40% of familial cases of HSCR and 3% to 7% of sporadic cases are associated with germline pathogenic variants in the RET proto-oncogene and are designated HSCR1.[71,72] Some of these RET pathogenic variants are more commonly located in codons that lead to the development of MEN2A or FMTC (i.e., codons 609, 618, and 620).[70,73] In a study of 44 families, seven families (16%) had cosegregation of MEN2A and HSCR1. The probability that individuals in a family with MEN2A and an exon 10 Cys variant would manifest HSCR1 was estimated to be 6% in one series.[71] Furthermore, in a multicenter international RET variant consortium study, 6 of 62 kindreds carrying either the C618R or C620R variant also had HSCR.[53] A novel analytic approach employing family-based association studies coupled with comparative and functional genomic analysis revealed that a common RETvariant within a conserved enhancer-like sequence in intron 1 makes a 20-fold greater contribution to HSCR compared with all known RET pathogenic variants.[74] This pathogenic variant has low penetrance and different genetic effects in males and females. Transmission to sons leads to a 5.7-fold increase in susceptibility and transmission to daughters leads to a 2.1-fold increase in susceptibility. This finding is consistent with the greater incidence of HSCR in males. Demonstrating this strong relationship between a common noncoding variant in RET and the risk of HSCR also accounts for previous failures to detect coding pathogenic variants in RET-linked families. Figure 2 depicts some of the classic manifestations of MEN2A in a family. 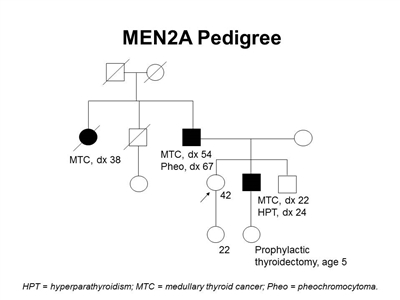
Figure 2. MEN2A pedigree. This pedigree shows some of the classic features of a family with a RET pathogenic variant across four generations, including affected family members with medullary thyroid cancer, pheochromocytoma, and hyperparathyroidism. Age at onset can vary widely, even within families. Medullary thyroid cancer can present with earlier onset and more aggressive disease in successive generations, depending on the genotype. MEN2A families may exhibit some or all of these features. As an autosomal dominant syndrome, transmission can occur through maternal or paternal lineages.
In a child, the presence of oral and ocular neuromas and/or a tall and lanky appearance may warrant further investigation.[75] Some authors have recommended referral to genetic counseling for an individual with MTC or any of the following features:[75,76] - Benign oral and submucosal neuromas.
- Elongated face and large lips.
- Ganglioneuromatosis.
- Inability to cry tears (biologic mechanism unknown).
Familial medullary thyroid carcinoma (FMTC) The FMTC subtype makes up 5% to 49% of MEN2 cases and is defined as families with four or more cases of MTC in the absence of PHEO or parathyroid adenoma/hyperplasia.[53,77] Families with two or three cases of MTC and incompletely documented screening for PHEO and parathyroid disease may actually represent MEN2A; it has been suggested that these families should be considered unclassified.[16,78] Misclassification of families with MEN2A as having FMTC (because of too-small family size or later onset of other manifestations of MEN2A) may result in overlooking the risk of PHEO, a disease with significant morbidity and mortality. For this reason, there is debate about whether FMTC represents a separate entity or is a variation of MEN2A in which there is a lack of or delay in the onset of the other (nonthyroidal) manifestations of the MEN2A syndrome.[79] Some authors recommended,[1] therefore, that patients thought to have pure FMTC also be screened for PHEO and hyperparathyroidism. Whether and how often to perform this screening are matters of ongoing debate. (Refer to the Screening at-risk individuals for PHEO and Screening at-risk individuals for hyperparathyroidism sections of this summary for more information.) MEN2B MEN2B is diagnosed clinically by the presence of mucosal neuromas of the lips and tongue, medullated corneal nerve fibers, distinctive facies with enlarged lips, an asthenic Marfanoid body habitus, and MTC.[80,81,82] The MEN2B subtype makes up about 5% of MEN2 cases. The MEN2B subtype was initially called mucosal neuroma syndrome or Wagenmann-Froboese syndrome.[83] MEN2B is characterized by the early development of an aggressive form of MTC in all patients.[83,84] Patients with MEN2B who do not undergo thyroidectomy at an early age (at approximately age 1 year) are likely to develop metastatic MTC at an early age. Before intervention with early risk-reducing thyroidectomy, the average age at death in patients with MEN2B was 21 years. PHEOs occur in about 50% of MEN2B cases; about half are multiple and often bilateral. Clinically apparent parathyroid disease is very uncommon.[53,85,86] Patients with MEN2B may be identified in infancy or early childhood by a distinctive facial appearance and the presence of mucosal neuromas on the anterior dorsal surface of the tongue, palate, or pharynx. The lips become prominent over time, and submucosal nodules may be present on the vermilion border of the lips. Neuromas of the eyelids may cause thickening and eversion of the upper eyelid margins. Prominent thickened corneal nerves may be seen by slit lamp examination. About 40% of patients have diffuse ganglioneuromatosis of the gastrointestinal tract. Associated symptoms include abdominal distension, megacolon, constipation, and diarrhea. About 75% of patients have a Marfanoid habitus, often with kyphoscoliosis or lordosis, joint laxity, and decreased subcutaneous fat. Proximal muscle wasting and weakness can also be seen.[81,82] Molecular Genetics of MEN2 MEN2 syndromes are the result of inherited pathogenic variants in the RET gene, located on chromosome region 10q11.2.[87,88,89] The RET gene is a proto-oncogene composed of 21 exons over 55 kilobase of genomic material.[90,91] RET encodes a receptor tyrosine kinase with extracellular, transmembrane, and intracellular domains. Details of RET receptor and ligand interaction in this signaling pathway have been reviewed.[92] Briefly, the extracellular domain consists of a calcium-binding cadherin-like region and a cysteine-rich region that interacts with one of four ligands identified to date. These ligands, e.g., glial cell line-derived neurotrophic factor (GDNF), neurturin, persephin, and artemin, also interact with one of four coreceptors in the GDNF-family receptor-alpha family.[92] The tyrosine kinase catalytic core is located in the intracellular domain, which causes downstream signaling events through a variety of second messenger molecules. Normal tissues contain transcripts of several lengths.[93,94,95] Genetic testing MEN2 is a well-defined hereditary cancer syndrome for which genetic testing is considered an important part of the management for at-risk family members. It meets the criteria related to indications for genetic testing for cancer susceptibility outlined by the American Society of Clinical Oncology in its most recent genetic testing policy statement.[96] At-risk individuals are defined as first-degree relatives (parents, siblings, and children) of a person known to have MEN2. Testing allows the identification of people with asymptomatic MEN2 who can be offered risk-reducing thyroidectomy and biochemical screening as preventive measures. A negative pathogenic variant analysis in at-risk relatives, however, is informative only after a disease-causing variant has been identified in an affected relative. (Refer to the PDQ summary on Cancer Genetics Risk Assessment and Counseling for more information.) Because early detection of at-risk individuals affects medical management, testing of children who have no symptoms is considered beneficial.[96,97] (Refer to the Genotype-Phenotype Correlations and Risk Stratification section of this summary for more information about clinical management of at-risk individuals.) Germline DNA testing for RET pathogenic variants is generally recommended to all individuals with a diagnosis of MTC, regardless of whether there is a personal or family history suggestive of MEN2.[22,98] Approximately 95% of patients with MEN2A or MEN2B will have an identifiable germline RET pathogenic variant.[53] For FMTC, the detection rate is slightly lower at 88%.[53] Between 1% and 10% of individuals with apparently sporadic MTC will carry a germline RET pathogenic variant, underscoring the importance of testing all individuals diagnosed with MTC.[17,18,19,20,99] There is no evidence for the involvement of other genetic loci, and all pathogenic variant-negative families analyzed to date have demonstrated linkage to the RET gene. For families that do not have a detectable pathogenic variant, clinical recommendations can be based on the clinical features in the affected individual and in the family. There is considerable diversity in the techniques used and the approach to RET pathogenic variant testing among the various laboratories that perform this procedure. Methods used to detect variants in RET include polymerase chain reaction (PCR) followed by restriction enzyme digestion of PCR products, heteroduplex analysis, single-stranded conformation polymorphism analysis, denaturing high-performance liquid chromatography, and DNA sequencing.[100,101,102,103] Most testing laboratories, at a minimum, offer testing using a targeted exon approach; that is, the laboratories look for variants in the exons that are most commonly found to carry variants (exons 10, 11, 13, 14, 15 and 16). Other laboratories offer testing for all exons. If targeted exon testing in a family with a high clinical suspicion for MEN2 is normal, sequencing of the remaining exons can then be performed. These differences in variant detection method and targeted versus full gene testing represent important considerations for selecting a laboratory to perform a test and in interpreting the test result. (Refer to the PDQ summary on Cancer Genetics Risk Assessment and Counseling for more information about clinical validity.) Genotype-Phenotype Correlations and Risk Stratification Genotype-phenotype correlations in MEN2 are well-established and have long been used to guide clinicians in making medical management recommendations. Several groups have developed pathogenic variant-stratification tables based on clinical phenotype, age of onset, and aggressiveness of MTC.[1,22,78] This classification strategy was first put forth after the Seventh International Workshop on MEN in 2001, which provided guidelines for the age of genetic testing and prophylactic thyroidectomy.[22] This stratification has been revised by the American Thyroid Association (ATA).[1,104] The specific pathogenic variants and their ATA classification are summarized in Table 5 below. The ATA's classification scheme has not been prospectively validated as a basis for clinical decision-making. ATA-Highest Risk (HST) (previously labeled ATA-D) pathogenic variants are the most aggressive and carry the highest risk of developing MTC.[1] This category includes those with MEN2B and RET codon M918T pathogenic variants and is associated with the youngest age at disease onset and the highest risk of mortality. ATA-High Risk (H) (previously called ATA-C) pathogenic variants, codons 634 and A883F, are associated with a slightly lower risk, yet the MTC in patients with these pathogenic variants is still quite aggressive and may present at an early age. Former ATA-levels A and B pathogenic variants are now combined into a single group called Moderate Risk (MOD) and are associated with a lower risk of aggressive MTC relative to the risk seen in carriers of ATA-HST and ATA-H pathogenic variants. However, the risk of MTC is still substantially elevated over the general population risk and consideration of risk-reducing thyroidectomy is warranted.[1] Common pathogenic variants in the ATA-MOD category include codons 609, 618, and 804. A European multicenter study of 207 carriers of RET pathogenic variants supported previous suggestions that some pathogenic variants are associated with early-onset disease. For example, this study found that individuals with the C634Y pathogenic variant developed MTC at a significantly younger age (mean 3.2 years; 95% confidence interval [CI], 1.2-5.4) than individuals with the C634R pathogenic variant (mean 6.9 years; 95% CI, 4.9-8.8). In the former group of patients, risk-reducing thyroidectomy warrants consideration before the age of 5 years. Although limited by small numbers, the same study did not support a need for risk-reducing thyroidectomy in asymptomatic carriers of pathogenic variants in codons 609, 630, 768, 790, 791, 804, or 891 before the age of 10 years or for central lymph node dissection before the age of 20 years.[105] Some authors suggest using these differences as the basis for decisions on the timing of risk-reducing thyroidectomy and the extent of surgery.[22] Two other studies have found conflicting results suggesting that the C634R pathogenic variant is associated with a higher penetrance of MTC-related PHEO and hyperparathyroidism and a higher likelihood of lymph node and distant metastases at an earlier age than is C634Y.[106] Additional studies in larger populations are needed to further clarify this issue. Others have advocated using basal and stimulated calcitonin levels as a basis for determining the appropriate timing of thyroidectomy.[107,108] Level of evidence (calcitonin level as a basis for the timing of thyroidectomy): 4aii Pathogenic variants at codons 883 and 918 have been seen only in MEN2B and are associated with the earliest age of onset and the most aggressive form of MTC.[109,110,111,112,113] Approximately 95% of individuals with MEN2B will have the M918T pathogenic variant.[109,110,111,114] As discussed above, 50% of individuals with MEN2B will develop PHEO but PHPT is rare. In addition to variants at codons 883 and 918, some individuals with an MEN2B-like phenotype have been found to carry two germline variants.[115,116,117,118,119] It is likely that as testing for RET becomes more common in clinical practice, additional double variant phenotypes will be described. Pathogenic variants at codon 634 (ATA-H) are by far the most frequent finding in families with MEN2A. One study of 477 RET carriers showed that 52.1% had the C634R pathogenic variant, 26.0% carried the C634Y pathogenic variant, and 9.1% had the C634G pathogenic variant.[53] In general, pathogenic variants at codon 634 are associated with PHEOs and PHPT.[53,120] Until recently, MEN2A with cutaneous lichen amyloidosis had been seen almost exclusively in patients with pathogenic variants at codon 634.[53,55,121] However, a recent report described MTC and cutaneous lichen amyloidosis in an individual previously thought to have FMTC due to a codon 804 pathogenic variant.[122] Codon 634 pathogenic variants have also been described in FMTC but are almost exclusively C634Y.[53] In summary, ATA-HST and ATA-H (previously levels D and C, respectively) pathogenic variants confer the highest risk of MTC (about 95% lifetime risk) with a more aggressive disease course. There is an increased risk of PHEO (up to 50%).[53,123] Individuals with codon 634 pathogenic variants (but not codon 883 or 918 variants) also have an increased risk of PHPT.[53] Moderate-risk variants located in exon 10 of the RET gene include variants at codons 609, 611, 618, 620, and 630. These variants involve cysteine residues in the extracellular domain of the RET protein and have been seen in families with MEN2A and those with MTC only (FMTC).[19,53,78,124,125,126,127,128] The risk of MTC in individuals with these pathogenic variants is approximately 95% to 100%; the risk of PHEO and hyperparathyroidism is lower than that seen in individuals with other moderate-risk pathogenic variants. In a large series of 518 probands with MTC undergoing RET testing, most individuals with codon 609, 611, 618, 620, or 630 variants had only MTC and no other features suggestive of MEN2. The authors attributed this to the relatively short follow-up time, incomplete screening of family members, or the method of ascertainment (population-based).[31] Another large study of 390 carriers of exon 10 pathogenic variants showed an age-related risk of PHEO for individuals carrying any exon 10 pathogenic variant of 23.1% by age 50 years and 33% by age 60 years. Overall prevalence of PHEO was 17%. This study reported a 3.9% risk of developing hyperparathyroidism by age 60 years.[129] Individuals with pathogenic variants previously classified as ATA-level A (now classified with ATA-level B as ATA-MOD, i.e., codons 321, 515, 533, 600, 603, 606, 531/9 base pair duplication, and 532 duplication) have a lower, albeit still elevated, lifetime risk of MTC. MTC associated with these pathogenic variants tends to follow a more indolent course and have a later age at onset, although there are several reports of individuals with these pathogenic variants who developed MTC before age 20 years.[53,130,131,132,133,134] Although PHEO and PHPT are not commonly associated with these pathogenic variants, they have been described.[134] Table 5. Genotype-Phenotype Correlations in Multiple Endocrine Neoplasia Type 2a| RETPathogenic variant | Exon | Risk of Aggressive MTC | Incidence of PHEO | Incidence of HPTH | Presence of CLA | Presence of HSCR |
|---|
| CLA = cutaneous lichen amyloidosis; HSCR = Hirschsprung disease; HPTH = hyperparathyroidism; MTC = medullary thyroid cancer; PHEO = pheochromocytoma. | | a Adapted from Wells et al.[1] | | G533C | 8 | Moderate | ~10% | - | N | N | | C609F/G/R/S/Y | 10 | Moderate | ~10%-30% | ~10% | N | Y | | C611F/G/S/Y/W | 10 | Moderate | ~10%-30% | ~10% | N | Y | | C618F/R/S | 10 | Moderate | ~10%-30% | ~10% | N | Y | | C620F/R/S | 10 | Moderate | ~10%-30% | ~10% | N | Y | | C630R/Y | 11 | Moderate | ~10%-30% | ~10% | N | N | | D631Y | 11 | Moderate | ~50% | - | N | N | | C634F/G/R/S/W/Y | 11 | High | ~50% | ~20%-30% | Y | N | | K666E | 11 | Moderate | ~10% | - | N | N | | E768D | 13 | Moderate | - | - | N | N | | L790F | 13 | Moderate | ~10% | - | N | N | | V804L | 14 | Moderate | ~10% | ~10% | N | N | | V804M | 14 | Moderate | ~10% | ~10% | Y | N | | A883F | 15 | High | ~50% | - | N | N | | S891A | 15 | Moderate | ~10% | ~10% | N | N | | R912P | 16 | Moderate | - | - | N | N | | M918T | 16 | Highest | ~50% | - | N | N | In addition to the pathogenic variants categorized in Table 5, a number of rare or novel RET variants have been described. Some of these represent pathogenic variants that lead to an FMTC or MEN2 phenotype. Others may represent low penetrance alleles or modifying alleles that confer only a modest risk of developing MTC. Still others may be benign polymorphisms of no clinical significance. For example, some studies demonstrate compelling evidence that RET variants p.Tyr791Phe and p.Ser649Leu are likely benign polymorphisms, based on equal frequencies among cases and healthy controls and co-occurrence with other disease-causing variants that co-segregate with disease in the family.[135,136] Therefore, carriers of these variants are not treated as having MEN2 syndrome and asymptomatic family members are generally not tested for these variants. Comprehensive testing of all hotspot variants in exons 8 and 10-16 may be performed to rule out any other RET pathogenic variants, and more extensive testing of other disease-related genes may be warranted because of a diagnosis of PHEO. (Refer to the Familial Pheochromocytoma and Paraganglioma Syndrome section of this summary for more information.) Research is ongoing into the role of neutral RET sequence variants in modifying the clinical presentation of patients with MEN2A. The presence of certain RET polymorphisms is being analyzed for its impact on the likelihood for development of PHEO, hyperparathyroidism, and metastatic involvement with MTC.[137,138,139] A variety of approaches, including segregation analyses, in silico analyses, association studies, and functional assays, can be employed to determine the functional and clinical significance of a given genetic variant. A publicly available RET variant online database repository was recently developed and includes a complete list of variants and their associated pathogenicity, phenotype, and other associated clinical information and literature references.[140] Surveillance Screening at-risk individuals for PHEO The presence of a functioning PHEO can be excluded by appropriate biochemical screening before thyroidectomy in any patient with MEN2A or MEN2B. However, childhood PHEOs are rare in MEN2.[1] The ATA recommends that annual screening for PHEO be considered by age 11 years in patients with ATA-HST or ATA-H RET pathogenic variants.[1] The ATA recommends that patients with ATA-MOD RET pathologic variants have periodic screening for PHEO beginning by age 16 years.[1] MRI or other imaging tests may be ordered only if the biochemical results are abnormal.[27,141] Studies of individuals with sporadic or hereditary PHEO (including, but not limited to, individuals with MEN2) have suggested that measurement of catecholamine metabolites, specifically plasma-free metanephrines and/or urinary fractionated metanephrines, provides a higher diagnostic sensitivity than urinary catecholamines because of the episodic nature of catecholamine excretion.[34,35,36,37,38,39,40,142] Several reviews provide a succinct summary of the biochemical diagnosis, localization, and management of PHEO.[40,143] In addition to surgery, there are other clinical situations in which patients with catecholamine excess face special risk. An example is the healthy at-risk female patient who becomes pregnant. Pregnancy, labor, or delivery may precipitate a hypertensive crisis in persons who carry an unrecognized PHEO. Pregnant patients who are found to have catecholamine excess require appropriate pharmacotherapy before delivery. Level of evidence: 5 Screening at-risk individuals for hyperparathyroidism MEN2-related hyperparathyroidism is generally associated with mild, often asymptomatic hypercalcemia early in the natural history of the disease, which, left untreated, may become symptomatic.[64] Childhood hyperparathyroidism is rare in MEN2. Three studies found the median age at diagnosis was about 38 years.[64,144,145] The ATA provides recommendations for annual screening for hyperparathyroidism,[1] with screening beginning by age 11 years in carriers of ATA-HST and ATA-H pathogenic variants and by age 16 years for carriers of ATA-MOD RET pathogenic variants.[1] Testing typically includes albumin-corrected calcium or ionized serum calcium with or without intact parathyroid hormone (PTH) measurement. Level of evidence: 5 Screening at-risk individuals in kindreds without an identifiableRETpathogenic variant Risk-reducing thyroidectomy is not routinely offered to at-risk individuals unless MEN2A is confirmed. The screening protocol for MTC in patients with MEN2A is annual calcitonin stimulation test; however, caution must be used in interpreting test results because CCH that is not a precursor to MTC occurs in about 5% of the population.[10,11,146] In addition, there is significant risk of false-negative test results in patients younger than 15 years.[11] Screening for PHEO and parathyroid disease is the same as described above. For patients at risk of FMTC, annual screening for MTC is the same as for patients with MEN2A. Level of evidence: 5 Interventions Risk-reducing thyroidectomy Risk-reducing thyroidectomy is the oncologic treatment of choice for patients with MEN2. Managing the central neck, including the lymph nodes and parathyroid glands, requires consideration of patient age, disease burden, and serum calcitonin levels. Selective autotransplantation of parathyroid glands that were devascularized during a prophylactic thyroidectomy and/or central neck clearance will provide equivalent outcomes to removal of all four parathyroid glands. This selective approach also significantly reduces the detrimental outcome of hypoparathyroidism.[147] The optimal timing of surgery, however, is controversial.[4] A multidisciplinary approach involving risk-benefit ratios, surgical expertise and outcomes, access to care for long-term follow-up, titration of thyroid hormone replacement therapy throughout life, and assessment of risk of surgical complications may be carefully considered with a pediatric endocrinologist, surgeon, primary care physician, and parents. In contrast, a prospective analysis of 84 carriers of the RET gene pathogenic variant found that basal and pentagastrin-stimulated calcitonin levels could be used to determine the timing of total thyroidectomy.[107] When the basal or stimulated calcitonin was greater than 10 pg/mL, total thyroidectomy and central neck dissection were strongly recommended. In this series, a basal calcitonin level lower than 60 pg/mL was always associated with an intrathyroidal MTC; none of the 56 patients who went to surgery had metastatic involvement. These findings suggest that surgery can be safely delayed in gene carriers of a RET pathogenic variant until basal or stimulated calcitonin is above 10 pg/mL, while still maintaining the ability to achieve a disease-free state (i.e., an undetectable basal and stimulated calcitonin 6-12 months after surgery). The benefits of this approach are particularly noteworthy in the younger population of gene carriers, as a delay in surgery until the patient is older may reduce the risk of surgical complications. While this approach is promising, pentagastrin is currently not available in the United States for stimulation testing. Although calcium may be used as a substitute for pentagastrin, it has not been widely validated. One series of 503 at-risk individuals with ATA-MOD category pathogenic variants (including codons 533, 609, 611, 618, 620, 791, and 804) reported cumulative penetrance rates, median time to MTC, and predictive value of preoperative calcitonin.[108] The risk of developing MTC by age 50 years ranged from 18% to 95%, depending on the codon, with codon 620 having the highest penetrance. Most patients with MTC had node-negative disease, confirming the more indolent disease course that has been previously reported with these pathogenic variants. Although an elevated preoperative calcitonin level strongly predicted presence of MTC, relatively high false-negative rates (low normal calcitonin levels with MTC) were noted for many of the codons. This information is useful when counseling carriers of pathogenic variants regarding surgical decisions. Another study has confirmed that calcitonin levels could be a useful approach to determine the timing of thyroidectomy.[148] This study utilized preoperative basal calcitonin levels and ultrasound findings to determine timing of prophylactic thyroidectomy in 24 RET pathogenic variant carriers, many of whom carried pathogenic variants in the highest risk level and had delayed surgery until after age 20 years. All 17 individuals who underwent surgery had elevated preoperative calcitonin levels on the fully-automated chemiluminescence immunoassay. Fifteen of 17 individuals had MTC, but only two had lymph node involvement and/or local tissue invasion, and 16 of 17 were disease free at 22 months. Two patients had CCH. Of note, only 6 of 15 individuals with MTC had elevated calcitonin levels using the radioimmunoassay. The study is limited by a small population of patients with low disease burden but suggests that some calcitonin assays may be more sensitive than others. In a study of biochemical screening in a large family with MEN2A performed before pathogenic variant analysis became available, 22 family members without evidence of clinical disease had elevated calcitonin and underwent thyroidectomy. During a mean follow-up period of 11 years, all remained free of clinical disease, and 3 out of 22 had transient elevation of postoperative calcitonin levels.[149] The use of biochemical screening is limited, however, by the lack of data on age-specific calcitonin levels in children younger than 3 years; caution should be used when interpreting these values in this age group.[1] A study of 93 patients with MEN2 from a Dutch tumor registry documented the importance of early prophylactic thyroidectomy.[150] This group of patients represented all known Dutch patients with hereditary MTC; most cases (67%) were codon 634 pathogenic variants; only 6% were MEN2B cases. Patients in this series were screened with either biochemical testing (pre-RET era) or RET pathogenic variant analysis. In both groups, patients underwent surgery at a later age, but the percentage from the pre-RET era was significantly higher (96% vs. 69%, P = .004). Older age at prophylactic thyroidectomy was significantly associated with a higher risk of postoperative persistent/recurrent disease. Although there is concern that young age at total thyroidectomy is associated with higher risk of surgical complications, this study found no such evidence. Two additional case series provide further data supporting early risk-reducing thyroidectomy following testing for RET pathogenic variants.[151,152] Cases reported in both series could reflect selection biases: one study reported 71 patients from a national registry who had been treated with thyroidectomy but did not specify how these patients were selected, whereas the other study reported 21 patients seen at a referral center.[151,152] In both studies, a series of children from families with MEN2 or FMTC who were found to have RET pathogenic variants were screened for CCH and treated with risk-reducing thyroidectomy. These studies documented MTC in 93% of patients with MEN2 and 77% of patients with FMTC. The larger study found a correlation between age and larger tumor size, nodal metastases, postoperative recurrence of disease, and mean basal calcitonin levels. Surgical complications were rare.[151] No studies have compared the outcome of thyroidectomy based on pathogenic variant testing with thyroidectomy based on biochemical screening. In one large series, 260 MEN2A patients aged 0 to 20 years were identified as having undergone either an early total thyroidectomy (ages 1-5 years, n = 42) or late thyroidectomy (ages 6-20 years, n = 218).[153] There was a significantly lower rate of invasive or metastatic MTC among those who underwent surgery at an early age (57%) than among those who underwent surgery at a late age (76%). Follow-up information was available on only 28% of the cohort, as a result of the limitations of study design, with a median follow-up of only 2 years for this nonsystematically selected subgroup. Persistent or recurrent disease was reported among 0 of 9 early-surgery patients, versus 21 of 65 late-surgery patients. Both findings are consistent with the hypothesis that patients undergoing surgery before age 6 years have a more favorable outcome, but the nature of the data prevents this from being a definitive conclusion. Finally, evidence suggested that individuals carrying codon 634 pathogenic variants were much more likely to present with invasive or metastatic MTC and to develop persistent or recurrent disease than were those harboring pathogenic variants in codons 804, 618, or 620. A study of young, clinically asymptomatic individuals with MEN2A sought to determine if early thyroidectomy could prevent or cure MTC.[154] This study included 50 consecutively identified carriers of RET pathogenic variants who underwent thyroidectomy at 19 years or younger. Preoperative screening for CCH included basal and stimulated calcitonin levels and postoperative follow-up consisted of annual physical exam and intermittent basal and stimulated calcitonin measurements. All 50 individuals had at least 5 years of follow-up. Although MTC was identified in 33 of 50 patients at the time of surgery, in 44 of 50 (88%) there was no evidence of persistent or recurrent disease at a mean of 7 years follow-up. Six patients had basal or stimulated calcitonin abnormalities thought to represent residual MTC. None of the 22 patients who underwent surgery before age 8 years had any evidence of MTC. The data suggested that there was a lower incidence of persistent or recurrent disease in patients who had thyroidectomy earlier in life (defined as younger than 8 years) and who had no evidence of lymph node metastases. Normal preoperative basal calcitonin does not exclude the possibility of the patient having MTC. In one study of 80 carriers of RET pathogenic variants, 14 carriers had normal calcitonin tests and eight of these patients had small foci of MTC discovered at thyroidectomy.[11] Another study confirmed these findings,[83] as 14 children had total thyroidectomy based on positive genetic testing for MEN2; MTC was present in 11 and only four had elevated stimulated calcitonin levels before surgery. Although basal calcitonin levels may not be able to identify all patients with MTC preoperatively, this test has utility as a predictor of postoperative remission, lymph node metastases, and distant metastases.[155] In one study of 224 patients from a single institution, preoperative basal calcitonin levels greater than 500 pg/mL predicted failure to achieve biochemical remission.[155] The authors of this study found that nodal metastases started appearing at basal calcitonin levels of 40 pg/mL (normal, <10 pg/mL). In node-positive patients, distant metastases emerged at basal calcitonin levels of 150 pg/mL to 400 pg/mL. Using current sensitive calcitonin assays, a study of 308 RET carriers found that a normal basal preoperative calcitonin excluded the presence of lymph node metastases (100% negative predictive value).[156] Therefore, the preoperative basal calcitonin level is a useful prognostic indicator and may help guide the surgical approach. Although thyroidectomy before biochemical evidence of disease (normal preoperative calcitonin) may reduce the risk of recurrent disease, continued monitoring for residual or recurrent MTC is still recommended.[1,157] One study found that 10% of patients with MEN2A undergoing thyroidectomy developed recurrent disease, based on an initially undetectable basal and stimulated calcitonin levels (<2 pg/mL) that became positive 5 to 10 years after surgery.[154] Only 2% of patients had residual disease after prophylactic surgery as assessed by a persistently elevated basal or stimulated calcitonin.[154] Questions remain concerning the natural history of MEN2. As more information is acquired, recommendations regarding the optimal age for thyroidectomy and the potential role for genetics and biochemical screening may change. For example, a case report documents MTC before age 5 years in two siblings with MEN2A.[158] Conversely, another case report documents onset of cancer in midlife or later in some families with FMTC and in elderly relatives who carry the FMTC genotype but have not developed cancer.[159] The possibility that certain pathogenic variants (e.g., Cys634) might convey a significantly worse prognosis, if confirmed, may permit tailoring intervention based on knowing the specific RET variant.[153] These clinical observations suggest that the natural history of the MEN2 syndromes is variable and could be subject to modifying effects related to specific RET pathogenic variants, other genes, behavioral factors, or environmental exposures. Level of evidence: 5 Treatment for MTC Standard treatment for adults with MTC is surgical removal of the entire thyroid gland, including the posterior capsule, and central lymph node dissection.[1] Children with M918T pathogenic variants may benefit from a thyroidectomy in the first year of life, perhaps in the first months of life.[1] The decision to perform a prophylactic central neck dissection is generally made based on whether the parathyroid glands can be identified and left in situ well vascularized and viable or autotransplanted.[1] Likewise, children with ATA-H category pathologic variants may undergo prophylactic thyroidectomy at age 5 years or earlier, based on the serum calcitonin levels. A central neck dissection is typically only performed if there is radiographic evidence of metastatic lymph node involvement or if the serum calcitonin level is higher than 40 pg/mL.[1] The ATA recommends that children in the ATA-MOD category have physical examination, sonography of the neck, and measurement of the serum calcitonin beginning around age 5 years.[1] The absence of an abnormal calcitonin may prompt continued measurement every 6 to 12 months. A multidisciplinary team caring for the patient, including the pediatrician and surgeon should determine the timing of surgery in conjunction with the child's parents based on the trend in serum calcitonin levels, ultrasonographic findings, preference of the family, and experience of the treating physicians.[1] The ATA recommends compartment-directed lymph node dissection for the following situations:[1] - No evidence of distant metastases and no evidence of neck nodal metastases by ultrasound exam: Prophylactic central neck dissection concomitant with initial thyroidectomy for biopsy-proven disease.
- Any nodal disease present (in either central or lateral neck): Compartment-oriented ipsilateral lateral neck dissection.
- Absence of contralateral lateral nodal metastases and a planned central and ipsilateral lateral neck dissection: Consider contralateral lateral neck dissection when basal calcitonin levels are greater than 200 pg/mL.
Patients who have had total thyroidectomy will require lifelong thyroid hormone replacement therapy. The dosing of medication is age-dependent and treatment may be initiated based on ideal body weight. For healthy adults 60 years and younger with no cardiac disease, a reasonable starting dose is 1.6 to 1.8 µg/kg given once daily.[160] Older patients may require 20% to 30% less thyroid hormone.[161] Children clear T4 more rapidly than adults and consequently require relatively higher replacement by body weight. Depending on the age of the child, replacement is typically between 2 to 6 µg/kg.[162] It is important to note, however, that replacement is preferred over suppressive therapy. Since C-cell tumors are not thyroid-stimulating hormone (TSH)-dependent for growth, the T4 therapy for MTC patients therefore may be adjusted to maintain a TSH within the normal reference range. Thyroglobulin measurement may also be useful for adjusting and maintaining TSH levels within a normal reference range to prevent additional regrowth of remnant thyroid tissue.[163] Further investigation is needed to better interpret how this information should guide management. There is no difference in survival between familial and sporadic forms of MTC when adjusted for clinicopathologic factors. Chemotherapy and radiation are not effective against this type of cancer,[4,164,165] although clinical trials (phases I-III) of various targeted molecular therapies are ongoing at selected centers. Some of these compounds have shown partial responses in a small percentage of patients, but most studies have demonstrated disease stability as the most favorable response.[166,167,168,169] The use of vandetanib and cabozantinib is approved by the U.S. Food and Drug Administration for adult patients with progressive metastatic MTC who are ineligible for surgery. A phase III study found that progression-free survival was longer in adults who received vandetanib than in those who received placebo.[170] A phase I/II study of children with MEN2B found an objective partial response rate of 47% with vandetanib.[171] A double-blind, phase III trial that compared cabozantinib with placebo in 330 patients with progressive MTC showed an improvement in median progression-free survival across all subgroups.[172] To date, neither cabozantinib nor vandetanib has demonstrated improved overall survival.[170,172] Future studies will likely focus on the development of new targeted therapies and the use of combination therapy in MTC. (Refer to NCI's List of Clinical Trials for more information about these trials. Refer to the PDQ summary on Thyroid Cancer Treatment for more information about the treatment of thyroid cancer.) Level of evidence: 5 Treatment for MEN2-related PHEO PHEO may be either unilateral or bilateral in patients with MEN2. Laparoscopic adrenalectomy is the recommended approach by some authorities for the treatment of unilateral PHEO.[1,22,104] The risks, benefits, and potential of life-threatening adrenal insufficiency should be considered at the time of the initial operative planning. If disease appears unilateral, the contralateral gland may develop metachronous disease in 17% to 72% of patients.[173,174] In one series, 23 patients with a unilateral PHEO and a macroscopically normal contralateral adrenal gland were treated initially with unilateral adrenalectomy.[175] A PHEO developed within the retained gland in 12 (52%) of these patients, occurring a mean of 11.9 years after initial surgery. During follow-up after unilateral adrenalectomy, no patient experienced a hypertensive crisis or other problems attributable to an undiagnosed PHEO. In contrast, 10 of 43 patients (23%) treated with bilateral adrenalectomy experienced at least one episode of acute adrenal insufficiency; one of these patients died. Unilateral adrenalectomy appears to represent a reasonable management strategy for unilateral PHEO in patients with MEN2.[1,176,177,178] Many suggest strongly considering a cortical-sparing technique, even at the initial operation for seemingly unilateral disease.[1,179] (Refer to the Interventions section in the Familial PHEO and Paraganglioma Syndrome section of this summary for more information.) Because of the risk of contralateral gland disease, periodic surveillance (serum or urinary catecholamine measurements) for the development of disease in the contralateral adrenal gland is recommended.[1] Regarding the operative approach, several studies examined the value of a posterior retroperitoneoscopic adrenalectomy and found it to be safe and effective, with very low mortality and a low rate of minor complications, and conversion to open or laparoscopic lateral surgery required in only 1.7% of cases.[180,181] This approach appears to be feasible and preferred, but extensive experience is needed.[173,182,183,184,185] Level of evidence: 4 Treatment for hyperparathyroidism Most patients with MEN2-related parathyroid disease are either asymptomatic or diagnosed incidentally at the time of thyroidectomy. Typically, the hypercalcemia (when present) is mild, although it may be associated with increased urinary excretion of calcium and nephrolithiasis. As a consequence, the indications for surgical intervention are generally similar to those recommended for patients with sporadic, primary hyperparathyroidism.[22] In general, fewer than four of the parathyroid glands are involved at the time of detected abnormalities in calcium metabolism.[1] Treatment of hyperparathyroidism typically employs some extent of surgical removal of the involved glands. Cure of hyperparathyroidism was achieved surgically in 89% of one large series of patients;[64] however, 22% of resected patients in this study developed postoperative hypoparathyroidism. Five patients (9%) had recurrent hyperparathyroidism. This series employed various surgical techniques, including total parathyroidectomy with autotransplantation to the nondominant forearm (4 of 11 patients [36%] developed postoperative hypoparathyroidism), subtotal parathyroidectomy (6 of 12 patients [50%] developed hypoparathyroidism), and resection only of glands that were macroscopically enlarged (3 of 29 patients [10%] developed hypoparathyroidism). These data indicate that excision of only those parathyroid glands that are enlarged appears to be sufficient in most cases. Some investigators have suggested using the MEN2 subtype to decide where to place the parathyroid glands that are identified at the time of thyroid surgery. For patients with MEN2B in whom the risk of parathyroid disease is quite low, the parathyroid glands may be left in the neck. For patients with MEN2A and FMTC, it is suggested that the glands be implanted in the nondominant forearm to minimize the need for further surgery on the neck after risk-reducing thyroidectomy and a central lymph node dissection.[1,186] All patients who have undergone parathyroid surgery with autotransplantation of parathyroid tissue may be monitored for hypoparathyroidism.[1,104,187,188] Medical therapy of hyperparathyroidism has gained popularity with the advent of calcimimetics, agents that sensitize the calcium-sensing receptors on the parathyroid glands to circulating calcium levels and thereby reduce circulating PTH levels. In a randomized, double-blind, placebo-controlled trial, cinacalcet hydrochloride was shown to induce sustained reduction in circulating calcium and PTH levels in patients with primary hyperparathyroidism.[189] In patients who are high-risk surgical candidates, those with recurrent hyperparathyroidism, or those in whom life expectancy is limited, medical therapy may be a viable alternative to a surgical approach.[1] Level of evidence: 5 Genetic Counseling Mode of inheritance All of the MEN2 subtypes are inherited in an autosomal dominant manner. For the child of someone with MEN2, the risk of inheriting the MEN2 pathogenic variant is 50%. Some individuals with MEN2, however, carry a de novo pathogenic variant; that is, they carry a new pathogenic variant that was not present in previous generations of their family and thus do not have an affected parent. The proportion of individuals with MEN2 who have an affected parent varies by subtype. MEN2A: About 95% of affected individuals have an affected parent. It is appropriate to evaluate the parents of an individual with MEN2A for manifestations of the disorder. In the 5% of cases that are not familial, either de novo pathogenic variants or incomplete penetrance of the mutant allele is possible.[190] FMTC: Multiple family members are affected; therefore, all affected individuals inherited the mutant gene from a parent. MEN2B: About 50% of affected individuals have de novo RET gene pathogenic variants, and 50% have inherited the pathogenic variant from a parent.[191,192] The majority of de novo pathogenic variants are paternal in origin, but cases of maternal origin have been reported.[193] Siblings of a proband: The risk to siblings depends on the genetic status of the parent, which can be clarified by pedigree analysis and/or DNA-based testing. In situations of apparent de novo pathogenic variants, germline mosaicism in an apparently unaffected parent must be considered, even though such an occurrence has not yet been reported. Attitudes toward preimplantation genetic diagnosis One study explored the attitudes of individuals with MEN1 and MEN2 toward preimplantation genetic diagnosis (PGD).[194] Ninety-one clinic-based patients from a single U.S. institution who had MEN1 and an MEN1 pathogenic variant or MEN2 and a RET pathogenic variant were surveyed. The study found that 30% (10 of 33) of those with MEN1 and 37% (21 of 57) of those with MEN2 were aware of PGD; 82% (27 of 33) of those with MEN1 and 61% (34 of 56) of those with MEN2 thought PGD should be offered; and 61% (19 of 31) of those with MEN1 and 43% (23 of 54) of those with MEN2 would consider PGD. Psychosocial issues The psychosocial impact of genetic testing for pathogenic variants in RET has not been extensively studied. Published studies have had limitations such as small sample size and heterogeneous populations; thus, the clinical relevance of these findings should be interpreted with caution. Identification as the carrier of a pathogenic variant may affect self-esteem, family relationships, and quality of life.[195] In addition, misconceptions about genetic disease may result in familial blame and guilt.[196,197] Several review articles outline both the medical and psychological issues, especially those related to the testing of children.[198,199,200,201] The medical value of early screening and risk-reducing treatment are contrasted with the loss of decision-making autonomy for the individual. Lack of agreement between parents about the value and timing of genetic testing and surgery may spur the development of emotional problems within the family. One study examined levels of psychological distress in the interval between submitting a blood sample and receiving genetic test results. Those individuals who experienced the highest level of distress were younger than 25 years, single, and had a history of responding to distressful situations with anxiety.[202] Pathogenic variant-positive parents whose children received negative test results did not seem to be reassured, questioned the reliability of the DNA test, and were eager to continue screening of their noncarrier children.[203] A small qualitative study (N = 21) evaluated how patients with MEN2A and family members conceptualized participation in lifelong high-risk surveillance.[204] Ongoing surveillance was viewed as a reminder of a health threat. Acceptance and incorporation of lifelong surveillance into routine health care was essential for coping with the implications of this condition. Concern about genetic predisposition to cancer was peripheral to concerns about surveillance. Supportive interventions, such as Internet discussion forums, can serve as an ongoing means of addressing informational and support needs of patients with MTC undergoing lifelong surveillance.[205] References:
-
Wells SA Jr, Asa SL, Dralle H, et al.: Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 25 (6): 567-610, 2015.
-
Kaserer K, Scheuba C, Neuhold N, et al.: Sporadic versus familial medullary thyroid microcarcinoma: a histopathologic study of 50 consecutive patients. Am J Surg Pathol 25 (10): 1245-51, 2001.
-
Robbins J, Merino MJ, Boice JD Jr, et al.: Thyroid cancer: a lethal endocrine neoplasm. Ann Intern Med 115 (2): 133-47, 1991.
-
Moley JF, Debenedetti MK, Dilley WG, et al.: Surgical management of patients with persistent or recurrent medullary thyroid cancer. J Intern Med 243 (6): 521-6, 1998.
-
Machens A, Lorenz K, Dralle H: Constitutive RET tyrosine kinase activation in hereditary medullary thyroid cancer: clinical opportunities. J Intern Med 266 (1): 114-25, 2009.
-
DeLellis RA, Lloyd RV, Heitz PU, et al., eds.: Pathology and Genetics of Tumours of Endocrine Organs. Lyon, France: IARC Press, 2004. World Health Organization classification of tumours, vol. 8.
-
Guyétant S, Rousselet MC, Durigon M, et al.: Sex-related C cell hyperplasia in the normal human thyroid: a quantitative autopsy study. J Clin Endocrinol Metab 82 (1): 42-7, 1997.
-
LiVolsi VA: C cell hyperplasia/neoplasia. J Clin Endocrinol Metab 82 (1): 39-41, 1997.
-
Mete O, Asa SL: Precursor lesions of endocrine system neoplasms. Pathology 45 (3): 316-30, 2013.
-
Landsvater RM, Rombouts AG, te Meerman GJ, et al.: The clinical implications of a positive calcitonin test for C-cell hyperplasia in genetically unaffected members of an MEN2A kindred. Am J Hum Genet 52 (2): 335-42, 1993.
-
Lips CJ, Landsvater RM, Höppener JW, et al.: Clinical screening as compared with DNA analysis in families with multiple endocrine neoplasia type 2A. N Engl J Med 331 (13): 828-35, 1994.
-
Elisei R, Bottici V, Luchetti F, et al.: Impact of routine measurement of serum calcitonin on the diagnosis and outcome of medullary thyroid cancer: experience in 10,864 patients with nodular thyroid disorders. J Clin Endocrinol Metab 89 (1): 163-8, 2004.
-
Kudo T, Miyauchi A, Ito Y, et al.: Serum calcitonin levels with calcium loading tests before and after total thyroidectomy in patients with thyroid diseases other than medullary thyroid carcinoma. Endocr J 58 (3): 217-21, 2011.
-
Incidence: Thyroid Cancer. Bethesda, Md: National Cancer Institute, SEER, 2004. Available online. Last accessed April 6, 2017.
-
Gharib H, McConahey WM, Tiegs RD, et al.: Medullary thyroid carcinoma: clinicopathologic features and long-term follow-up of 65 patients treated during 1946 through 1970. Mayo Clin Proc 67 (10): 934-40, 1992.
-
Ponder BA: Multiple endocrine neoplasia type 2. In: Vogelstein B, Kinzler KW, eds.: The Genetic Basis of Human Cancer. 2nd ed. New York, NY: McGraw-Hill, 2002, pp 501-513.
-
Decker RA, Peacock ML, Borst MJ, et al.: Progress in genetic screening of multiple endocrine neoplasia type 2A: is calcitonin testing obsolete? Surgery 118 (2): 257-63; discussion 263-4, 1995.
-
Kitamura Y, Goodfellow PJ, Shimizu K, et al.: Novel germline RET proto-oncogene mutations associated with medullary thyroid carcinoma (MTC): mutation analysis in Japanese patients with MTC. Oncogene 14 (25): 3103-6, 1997.
-
Eng C, Mulligan LM, Smith DP, et al.: Low frequency of germline mutations in the RET proto-oncogene in patients with apparently sporadic medullary thyroid carcinoma. Clin Endocrinol (Oxf) 43 (1): 123-7, 1995.
-
Wohllk N, Cote GJ, Bugalho MM, et al.: Relevance of RET proto-oncogene mutations in sporadic medullary thyroid carcinoma. J Clin Endocrinol Metab 81 (10): 3740-5, 1996.
-
Lips CJ: Clinical management of the multiple endocrine neoplasia syndromes: results of a computerized opinion poll at the Sixth International Workshop on Multiple Endocrine Neoplasia and von Hippel-Lindau disease. J Intern Med 243 (6): 589-94, 1998.
-
Brandi ML, Gagel RF, Angeli A, et al.: Guidelines for diagnosis and therapy of MEN type 1 and type 2. J Clin Endocrinol Metab 86 (12): 5658-71, 2001.
-
National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology: Thyroid Carcinoma. Version 2.2015. Fort Washington, Pa: National Comprehensive Cancer Network, 2015. Available online with free subscription. Last accessed April 6, 2017.
-
American Cancer Society: Cancer Facts and Figures 2017. Atlanta, Ga: American Cancer Society, 2017. Available online. Last accessed May 25, 2017.
-
Hundahl SA, Fleming ID, Fremgen AM, et al.: A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985-1995 [see comments] Cancer 83 (12): 2638-48, 1998.
-
Bhattacharyya N: A population-based analysis of survival factors in differentiated and medullary thyroid carcinoma. Otolaryngol Head Neck Surg 128 (1): 115-23, 2003.
-
Modigliani E, Vasen HM, Raue K, et al.: Pheochromocytoma in multiple endocrine neoplasia type 2: European study. The Euromen Study Group. J Intern Med 238 (4): 363-7, 1995.
-
Roman S, Lin R, Sosa JA: Prognosis of medullary thyroid carcinoma: demographic, clinical, and pathologic predictors of survival in 1252 cases. Cancer 107 (9): 2134-42, 2006.
-
Bergholm U, Bergström R, Ekbom A: Long-term follow-up of patients with medullary carcinoma of the thyroid. Cancer 79 (1): 132-8, 1997.
-
Kebebew E, Ituarte PH, Siperstein AE, et al.: Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems. Cancer 88 (5): 1139-48, 2000.
-
Elisei R, Romei C, Cosci B, et al.: RET genetic screening in patients with medullary thyroid cancer and their relatives: experience with 807 individuals at one center. J Clin Endocrinol Metab 92 (12): 4725-9, 2007.
-
Paszko Z, Sromek M, Czetwertynska M, et al.: The occurrence and the type of germline mutations in the RET gene in patients with medullary thyroid carcinoma and their unaffected kindred's from Central Poland. Cancer Invest 25 (8): 742-9, 2007.
-
Pelizzo MR, Boschin IM, Bernante P, et al.: Natural history, diagnosis, treatment and outcome of medullary thyroid cancer: 37 years experience on 157 patients. Eur J Surg Oncol 33 (4): 493-7, 2007.
-
Lenders JW, Pacak K, Walther MM, et al.: Biochemical diagnosis of pheochromocytoma: which test is best? JAMA 287 (11): 1427-34, 2002.
-
Gerlo EA, Sevens C: Urinary and plasma catecholamines and urinary catecholamine metabolites in pheochromocytoma: diagnostic value in 19 cases. Clin Chem 40 (2): 250-6, 1994.
-
Guller U, Turek J, Eubanks S, et al.: Detecting pheochromocytoma: defining the most sensitive test. Ann Surg 243 (1): 102-7, 2006.
-
Raber W, Raffesberg W, Bischof M, et al.: Diagnostic efficacy of unconjugated plasma metanephrines for the detection of pheochromocytoma. Arch Intern Med 160 (19): 2957-63, 2000.
-
Sawka AM, Jaeschke R, Singh RJ, et al.: A comparison of biochemical tests for pheochromocytoma: measurement of fractionated plasma metanephrines compared with the combination of 24-hour urinary metanephrines and catecholamines. J Clin Endocrinol Metab 88 (2): 553-8, 2003.
-
Unger N, Pitt C, Schmidt IL, et al.: Diagnostic value of various biochemical parameters for the diagnosis of pheochromocytoma in patients with adrenal mass. Eur J Endocrinol 154 (3): 409-17, 2006.
-
Pacak K, Eisenhofer G, Ahlman H, et al.: Pheochromocytoma: recommendations for clinical practice from the First International Symposium. October 2005. Nat Clin Pract Endocrinol Metab 3 (2): 92-102, 2007.
-
van der Harst E, de Herder WW, Bruining HA, et al.: [(123)I]metaiodobenzylguanidine and [(111)In]octreotide uptake in begnign and malignant pheochromocytomas. J Clin Endocrinol Metab 86 (2): 685-93, 2001.
-
Pacak K, Linehan WM, Eisenhofer G, et al.: Recent advances in genetics, diagnosis, localization, and treatment of pheochromocytoma. Ann Intern Med 134 (4): 315-29, 2001.
-
Kaelin WG Jr: Molecular basis of the VHL hereditary cancer syndrome. Nat Rev Cancer 2 (9): 673-82, 2002.
-
Maher ER, Eng C: The pressure rises: update on the genetics of phaeochromocytoma. Hum Mol Genet 11 (20): 2347-54, 2002.
-
Neumann HP, Bausch B, McWhinney SR, et al.: Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med 346 (19): 1459-66, 2002.
-
Amar L, Bertherat J, Baudin E, et al.: Genetic testing in pheochromocytoma or functional paraganglioma. J Clin Oncol 23 (34): 8812-8, 2005.
-
Gimenez-Roqueplo AP, Lehnert H, Mannelli M, et al.: Phaeochromocytoma, new genes and screening strategies. Clin Endocrinol (Oxf) 65 (6): 699-705, 2006.
-
Fraser WD: Hyperparathyroidism. Lancet 374 (9684): 145-58, 2009.
-
Tonelli F, Marcucci T, Giudici F, et al.: Surgical approach in hereditary hyperparathyroidism. Endocr J 56 (7): 827-41, 2009.
-
Villablanca A, Calender A, Forsberg L, et al.: Germline and de novo mutations in the HRPT2 tumour suppressor gene in familial isolated hyperparathyroidism (FIHP). J Med Genet 41 (3): e32, 2004.
-
Marx SJ, Simonds WF, Agarwal SK, et al.: Hyperparathyroidism in hereditary syndromes: special expressions and special managements. J Bone Miner Res 17 (Suppl 2): N37-43, 2002.
-
Sipple JH: The association of pheochromocytoma with carcinoma of the thyroid gland. Am J Med 31 (1): 163-166, 1961.
-
Eng C, Clayton D, Schuffenecker I, et al.: The relationship between specific RET proto-oncogene mutations and disease phenotype in multiple endocrine neoplasia type 2. International RET mutation consortium analysis. JAMA 276 (19): 1575-9, 1996.
-
Sanso GE, Domene HM, Garcia R, et al.: Very early detection of RET proto-oncogene mutation is crucial for preventive thyroidectomy in multiple endocrine neoplasia type 2 children: presence of C-cell malignant disease in asymptomatic carriers. Cancer 94 (2): 323-30, 2002.
-
Yip L, Cote GJ, Shapiro SE, et al.: Multiple endocrine neoplasia type 2: evaluation of the genotype-phenotype relationship. Arch Surg 138 (4): 409-16; discussion 416, 2003.
-
Rambaud JC, Jian R, Flourié B, et al.: Pathophysiological study of diarrhoea in a patient with medullary thyroid carcinoma. Evidence against a secretory mechanism and for the role of shortened colonic transit time. Gut 29 (4): 537-43, 1988.
-
Cox TM, Fagan EA, Hillyard CJ, et al.: Rôle of calcitonin in diarrhoea associated with medullary carcinoma of the thyroid. Gut 20 (7): 629-33, 1979.
-
Raue F, Frank-Raue K, Grauer A: Multiple endocrine neoplasia type 2. Clinical features and screening. Endocrinol Metab Clin North Am 23 (1): 137-56, 1994.
-
Perren A, Komminoth P: Familial pheochromocytomas and paragangliomas: stories from the sign-out room. Endocr Pathol 17 (4): 337-44, 2006.
-
Webb TA, Sheps SG, Carney JA: Differences between sporadic pheochromocytoma and pheochromocytoma in multiple endocrime neoplasia, type 2. Am J Surg Pathol 4 (2): 121-6, 1980.
-
Lips KJ, Van der Sluys Veer J, Struyvenberg A, et al.: Bilateral occurrence of pheochromocytoma in patients with the multiple endocrine neoplasia syndrome type 2A (Sipple's syndrome). Am J Med 70 (5): 1051-60, 1981.
-
Neumann HP, Berger DP, Sigmund G, et al.: Pheochromocytomas, multiple endocrine neoplasia type 2, and von Hippel-Lindau disease. N Engl J Med 329 (21): 1531-8, 1993.
-
Conte-Devolx B, Schuffenecker I, Niccoli P, et al.: Multiple endocrine neoplasia type 2: management of patients and subjects at risk. French Study Group on Calcitonin-Secreting Tumors (GETC). Horm Res 47 (4-6): 221-6, 1997.
-
Kraimps JL, Denizot A, Carnaille B, et al.: Primary hyperparathyroidism in multiple endocrine neoplasia type IIa: retrospective French multicentric study. Groupe d'Etude des Tumeurs á Calcitonine (GETC, French Calcitonin Tumors Study Group), French Association of Endocrine Surgeons. World J Surg 20 (7): 808-12; discussion 812-3, 1996.
-
Benson L, Ljunghall S, Akerström G, et al.: Hyperparathyroidism presenting as the first lesion in multiple endocrine neoplasia type 1. Am J Med 82 (4): 731-7, 1987.
-
Trump D, Farren B, Wooding C, et al.: Clinical studies of multiple endocrine neoplasia type 1 (MEN1) QJM 89 (9): 653-69, 1996.
-
Vasen HF, Lamers CB, Lips CJ: Screening for the multiple endocrine neoplasia syndrome type I. A study of 11 kindreds in The Netherlands. Arch Intern Med 149 (12): 2717-22, 1989.
-
Bugalho MJ, Limbert E, Sobrinho LG, et al.: A kindred with multiple endocrine neoplasia type 2A associated with pruritic skin lesions. Cancer 70 (11): 2664-7, 1992.
-
Robinson MF, Furst EJ, Nunziata V, et al.: Characterization of the clinical features of five families with hereditary primary cutaneous lichen amyloidosis and multiple endocrine neoplasia type 2. Henry Ford Hosp Med J 40 (3-4): 249-52, 1992.
-
Romeo G, Ceccherini I, Celli J, et al.: Association of multiple endocrine neoplasia type 2 and Hirschsprung disease. J Intern Med 243 (6): 515-20, 1998.
-
Decker RA, Peacock ML, Watson P: Hirschsprung disease in MEN 2A: increased spectrum of RET exon 10 genotypes and strong genotype-phenotype correlation. Hum Mol Genet 7 (1): 129-34, 1998.
-
Carrasquillo MM, McCallion AS, Puffenberger EG, et al.: Genome-wide association study and mouse model identify interaction between RET and EDNRB pathways in Hirschsprung disease. Nat Genet 32 (2): 237-44, 2002.
-
Mulligan LM, Eng C, Attié T, et al.: Diverse phenotypes associated with exon 10 mutations of the RET proto-oncogene. Hum Mol Genet 3 (12): 2163-7, 1994.
-
Emison ES, McCallion AS, Kashuk CS, et al.: A common sex-dependent mutation in a RET enhancer underlies Hirschsprung disease risk. Nature 434 (7035): 857-63, 2005.
-
Hampel H, Bennett RL, Buchanan A, et al.: A practice guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: referral indications for cancer predisposition assessment. Genet Med 17 (1): 70-87, 2015.
-
Brauckhoff M, Machens A, Hess S, et al.: Premonitory symptoms preceding metastatic medullary thyroid cancer in MEN 2B: An exploratory analysis. Surgery 144 (6): 1044-50; discussion 1050-3, 2008.
-
Romei C, Tacito A, Molinaro E, et al.: Twenty years of lesson learning: how does the RET genetic screening test impact the clinical management of medullary thyroid cancer? Clin Endocrinol (Oxf) 82 (6): 892-9, 2015.
-
Kouvaraki MA, Shapiro SE, Perrier ND, et al.: RET proto-oncogene: a review and update of genotype-phenotype correlations in hereditary medullary thyroid cancer and associated endocrine tumors. Thyroid 15 (6): 531-44, 2005.
-
Pacini F, Castagna MG, Cipri C, et al.: Medullary thyroid carcinoma. Clin Oncol (R Coll Radiol) 22 (6): 475-85, 2010.
-
Morrison PJ, Nevin NC: Multiple endocrine neoplasia type 2B (mucosal neuroma syndrome, Wagenmann-Froboese syndrome). J Med Genet 33 (9): 779-82, 1996.
-
Gorlin RJ, Sedano HO, Vickers RA, et al.: Multiple mucosal neuromas, pheochromocytoma and medullary carcinoma of the thyroid--a syndrome. Cancer 22 (2): 293-9 passim, 1968.
-
Gorlin RJ, Vickers RA: Multiple mucosal neuromas, pheochromocytoma, medullary carcinoma of the thyroid and marfanoid body build with muscle wasting: reexamination of a syndrome of neural crest malmigration. Birth Defects Orig Artic Ser 7 (6): 69-72, 1971.
-
Skinner MA, DeBenedetti MK, Moley JF, et al.: Medullary thyroid carcinoma in children with multiple endocrine neoplasia types 2A and 2B. J Pediatr Surg 31 (1): 177-81; discussion 181-2, 1996.
-
O'Riordain DS, O'Brien T, Weaver AL, et al.: Medullary thyroid carcinoma in multiple endocrine neoplasia types 2A and 2B. Surgery 116 (6): 1017-23, 1994.
-
Eng C: Seminars in medicine of the Beth Israel Hospital, Boston. The RET proto-oncogene in multiple endocrine neoplasia type 2 and Hirschsprung's disease. N Engl J Med 335 (13): 943-51, 1996.
-
Vasen HF, van der Feltz M, Raue F, et al.: The natural course of multiple endocrine neoplasia type IIb. A study of 18 cases. Arch Intern Med 152 (6): 1250-2, 1992.
-
Gardner E, Papi L, Easton DF, et al.: Genetic linkage studies map the multiple endocrine neoplasia type 2 loci to a small interval on chromosome 10q11.2. Hum Mol Genet 2 (3): 241-6, 1993.
-
Mole SE, Mulligan LM, Healey CS, et al.: Localisation of the gene for multiple endocrine neoplasia type 2A to a 480 kb region in chromosome band 10q11.2. Hum Mol Genet 2 (3): 247-52, 1993.
-
Takahashi M, Ritz J, Cooper GM: Activation of a novel human transforming gene, ret, by DNA rearrangement. Cell 42 (2): 581-8, 1985.
-
Kwok JB, Gardner E, Warner JP, et al.: Structural analysis of the human ret proto-oncogene using exon trapping. Oncogene 8 (9): 2575-82, 1993.
-
Myers SM, Eng C, Ponder BA, et al.: Characterization of RET proto-oncogene 3' splicing variants and polyadenylation sites: a novel C-terminus for RET. Oncogene 11 (10): 2039-45, 1995.
-
Airaksinen MS, Saarma M: The GDNF family: signalling, biological functions and therapeutic value. Nat Rev Neurosci 3 (5): 383-94, 2002.
-
Takaya K, Yoshimasa T, Arai H, et al.: Expression of the RET proto-oncogene in normal human tissues, pheochromocytomas, and other tumors of neural crest origin. J Mol Med 74 (10): 617-21, 1996.
-
Kurokawa K, Kawai K, Hashimoto M, et al.: Cell signalling and gene expression mediated by RET tyrosine kinase. J Intern Med 253 (6): 627-33, 2003.
-
Manié S, Santoro M, Fusco A, et al.: The RET receptor: function in development and dysfunction in congenital malformation. Trends Genet 17 (10): 580-9, 2001.
-
Robson ME, Storm CD, Weitzel J, et al.: American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol 28 (5): 893-901, 2010.
-
Points to consider: ethical, legal, and psychosocial implications of genetic testing in children and adolescents. American Society of Human Genetics Board of Directors, American College of Medical Genetics Board of Directors. Am J Hum Genet 57 (5): 1233-41, 1995.
-
Cooper DS, Doherty GM, Haugen BR, et al.: Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19 (11): 1167-214, 2009.
-
Sarika HL, Papathoma A, Garofalaki M, et al.: Genetic screening of patients with medullary thyroid cancer in a referral center in Greece during the past two decades. Eur J Endocrinol 172 (4): 501-9, 2015.
-
Ceccherini I, Hofstra RM, Luo Y, et al.: DNA polymorphisms and conditions for SSCP analysis of the 20 exons of the ret proto-oncogene. Oncogene 9 (10): 3025-9, 1994.
-
Xue F, Yu H, Maurer LH, et al.: Germline RET mutations in MEN 2A and FMTC and their detection by simple DNA diagnostic tests. Hum Mol Genet 3 (4): 635-8, 1994.
-
McMahon R, Mulligan LM, Healey CS, et al.: Direct, non-radioactive detection of mutations in multiple endocrine neoplasia type 2A families. Hum Mol Genet 3 (4): 643-6, 1994.
-
Kambouris M, Jackson CE, Feldman GL: Diagnosis of multiple endocrine neoplasia [MEN] 2A, 2B and familial medullary thyroid cancer [FMTC] by multiplex PCR and heteroduplex analyses of RET proto-oncogene mutations. Hum Mutat 8 (1): 64-70, 1996.
-
Kloos RT, Eng C, Evans DB, et al.: Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid 19 (6): 565-612, 2009.
-
Machens A, Niccoli-Sire P, Hoegel J, et al.: Early malignant progression of hereditary medullary thyroid cancer. N Engl J Med 349 (16): 1517-25, 2003.
-
Valdés N, Navarro E, Mesa J, et al.: RET Cys634Arg mutation confers a more aggressive multiple endocrine neoplasia type 2A phenotype than Cys634Tyr mutation. Eur J Endocrinol 172 (3): 301-7, 2015.
-
Elisei R, Romei C, Renzini G, et al.: The timing of total thyroidectomy in RET gene mutation carriers could be personalized and safely planned on the basis of serum calcitonin: 18 years experience at one single center. J Clin Endocrinol Metab 97 (2): 426-35, 2012.
-
Rich TA, Feng L, Busaidy N, et al.: Prevalence by age and predictors of medullary thyroid cancer in patients with lower risk germline RET proto-oncogene mutations. Thyroid 24 (7): 1096-106, 2014.
-
Eng C, Smith DP, Mulligan LM, et al.: Point mutation within the tyrosine kinase domain of the RET proto-oncogene in multiple endocrine neoplasia type 2B and related sporadic tumours. Hum Mol Genet 3 (2): 237-41, 1994.
-
Hofstra RM, Landsvater RM, Ceccherini I, et al.: A mutation in the RET proto-oncogene associated with multiple endocrine neoplasia type 2B and sporadic medullary thyroid carcinoma. Nature 367 (6461): 375-6, 1994.
-
Carlson KM, Dou S, Chi D, et al.: Single missense mutation in the tyrosine kinase catalytic domain of the RET protooncogene is associated with multiple endocrine neoplasia type 2B. Proc Natl Acad Sci U S A 91 (4): 1579-83, 1994.
-
Gimm O, Marsh DJ, Andrew SD, et al.: Germline dinucleotide mutation in codon 883 of the RET proto-oncogene in multiple endocrine neoplasia type 2B without codon 918 mutation. J Clin Endocrinol Metab 82 (11): 3902-4, 1997.
-
Smith DP, Houghton C, Ponder BA: Germline mutation of RET codon 883 in two cases of de novo MEN 2B. Oncogene 15 (10): 1213-7, 1997.
-
Eng C, Mulligan LM, Healey CS, et al.: Heterogeneous mutation of the RET proto-oncogene in subpopulations of medullary thyroid carcinoma. Cancer Res 56 (9): 2167-70, 1996.
-
Cranston AN, Carniti C, Oakhill K, et al.: RET is constitutively activated by novel tandem mutations that alter the active site resulting in multiple endocrine neoplasia type 2B. Cancer Res 66 (20): 10179-87, 2006.
-
Miyauchi A, Futami H, Hai N, et al.: Two germline missense mutations at codons 804 and 806 of the RET proto-oncogene in the same allele in a patient with multiple endocrine neoplasia type 2B without codon 918 mutation. Jpn J Cancer Res 90 (1): 1-5, 1999.
-
Kameyama K, Okinaga H, Takami H: RET oncogene mutations in 75 cases of familial medullary thyroid carcinoma in Japan. Biomed Pharmacother 58 (6-7): 345-7, 2004 Jul-Aug.
-
Iwashita T, Murakami H, Kurokawa K, et al.: A two-hit model for development of multiple endocrine neoplasia type 2B by RET mutations. Biochem Biophys Res Commun 268 (3): 804-8, 2000.
-
Menko FH, van der Luijt RB, de Valk IA, et al.: Atypical MEN type 2B associated with two germline RET mutations on the same allele not involving codon 918. J Clin Endocrinol Metab 87 (1): 393-7, 2002.
-
Mulligan LM, Eng C, Healey CS, et al.: Specific mutations of the RET proto-oncogene are related to disease phenotype in MEN 2A and FMTC. Nat Genet 6 (1): 70-4, 1994.
-
Seri M, Celli I, Betsos N, et al.: A Cys634Gly substitution of the RET proto-oncogene in a family with recurrence of multiple endocrine neoplasia type 2A and cutaneous lichen amyloidosis. Clin Genet 51 (2): 86-90, 1997.
-
Rothberg AE, Raymond VM, Gruber SB, et al.: Familial medullary thyroid carcinoma associated with cutaneous lichen amyloidosis. Thyroid 19 (6): 651-5, 2009.
-
Quayle FJ, Fialkowski EA, Benveniste R, et al.: Pheochromocytoma penetrance varies by RET mutation in MEN 2A. Surgery 142 (6): 800-5; discussion 805.e1, 2007.
-
Bolino A, Schuffenecker I, Luo Y, et al.: RET mutations in exons 13 and 14 of FMTC patients. Oncogene 10 (12): 2415-9, 1995.
-
Boccia LM, Green JS, Joyce C, et al.: Mutation of RET codon 768 is associated with the FMTC phenotype. Clin Genet 51 (2): 81-5, 1997.
-
Lesueur F, Cebrian A, Cranston A, et al.: Germline homozygous mutations at codon 804 in the RET protooncogene in medullary thyroid carcinoma/multiple endocrine neoplasia type 2A patients. J Clin Endocrinol Metab 90 (6): 3454-7, 2005.
-
Shannon KE, Gimm O, Hinze R: Germline V804M mutation in the RET protooncogene in 2 apparently sporadic cases of MTC presenting in the 7th decade of life. The Journal of Endocrine Genetics 1 (1): 39-46, 1999.
-
Raue F, Frank-Raue K: Genotype-phenotype relationship in multiple endocrine neoplasia type 2. Implications for clinical management. Hormones (Athens) 8 (1): 23-8, 2009 Jan-Mar.
-
Frank-Raue K, Rybicki LA, Erlic Z, et al.: Risk profiles and penetrance estimations in multiple endocrine neoplasia type 2A caused by germline RET mutations located in exon 10. Hum Mutat 32 (1): 51-8, 2011.
-
Mulligan LM, Marsh DJ, Robinson BG, et al.: Genotype-phenotype correlation in multiple endocrine neoplasia type 2: report of the International RET Mutation Consortium. J Intern Med 238 (4): 343-6, 1995.
-
Moers AM, Landsvater RM, Schaap C, et al.: Familial medullary thyroid carcinoma: not a distinct entity? Genotype-phenotype correlation in a large family. Am J Med 101 (6): 635-41, 1996.
-
Niccoli-Sire P, Murat A, Rohmer V, et al.: Familial medullary thyroid carcinoma with noncysteine ret mutations: phenotype-genotype relationship in a large series of patients. J Clin Endocrinol Metab 86 (8): 3746-53, 2001.
-
Machens A, Ukkat J, Brauckhoff M, et al.: Advances in the management of hereditary medullary thyroid cancer. J Intern Med 257 (1): 50-9, 2005.
-
Mukherjee S, Zakalik D: RET codon 804 mutations in multiple endocrine neoplasia 2: genotype-phenotype correlations and implications in clinical management. Clin Genet 79 (1): 1-16, 2011.
-
Erlic Z, Hoffmann MM, Sullivan M, et al.: Pathogenicity of DNA variants and double mutations in multiple endocrine neoplasia type 2 and von Hippel-Lindau syndrome. J Clin Endocrinol Metab 95 (1): 308-13, 2010.
-
Toledo RA, Hatakana R, Lourenço DM Jr, et al.: Comprehensive assessment of the disputed RET Y791F variant shows no association with medullary thyroid carcinoma susceptibility. Endocr Relat Cancer 22 (1): 65-76, 2015.
-
Siqueira DR, Ceolin L, Ferreira CV, et al.: Role of RET genetic variants in MEN2-associated pheochromocytoma. Eur J Endocrinol 170 (6): 821-8, 2014.
-
Ceolin L, Siqueira DR, Romitti M, et al.: Molecular basis of medullary thyroid carcinoma: the role of RET polymorphisms. Int J Mol Sci 13 (1): 221-39, 2012.
-
Robledo M, Gil L, Pollán M, et al.: Polymorphisms G691S/S904S of RET as genetic modifiers of MEN 2A. Cancer Res 63 (8): 1814-7, 2003.
-
Margraf RL, Crockett DK, Krautscheid PM, et al.: Multiple endocrine neoplasia type 2 RET protooncogene database: repository of MEN2-associated RET sequence variation and reference for genotype/phenotype correlations. Hum Mutat 30 (4): 548-56, 2009.
-
Wells SA Jr, Donis-Keller H: Current perspectives on the diagnosis and management of patients with multiple endocrine neoplasia type 2 syndromes. Endocrinol Metab Clin North Am 23 (1): 215-28, 1994.
-
Gardet V, Gatta B, Simonnet G, et al.: Lessons from an unpleasant surprise: a biochemical strategy for the diagnosis of pheochromocytoma. J Hypertens 19 (6): 1029-35, 2001.
-
Pacak K, Ilias I, Adams KT, et al.: Biochemical diagnosis, localization and management of pheochromocytoma: focus on multiple endocrine neoplasia type 2 in relation to other hereditary syndromes and sporadic forms of the tumour. J Intern Med 257 (1): 60-8, 2005.
-
Raue F, Kraimps JL, Dralle H, et al.: Primary hyperparathyroidism in multiple endocrine neoplasia type 2A. J Intern Med 238 (4): 369-73, 1995.
-
Milos IN, Frank-Raue K, Wohllk N, et al.: Age-related neoplastic risk profiles and penetrance estimations in multiple endocrine neoplasia type 2A caused by germ line RET Cys634Trp (TGC>TGG) mutation. Endocr Relat Cancer 15 (4): 1035-41, 2008.
-
Marsh DJ, McDowall D, Hyland VJ, et al.: The identification of false positive responses to the pentagastrin stimulation test in RET mutation negative members of MEN 2A families. Clin Endocrinol (Oxf) 44 (2): 213-20, 1996.
-
Moley JF, Skinner M, Gillanders WE, et al.: Management of the Parathyroid Glands During Preventive Thyroidectomy in Patients With Multiple Endocrine Neoplasia Type 2. Ann Surg 262 (4): 641-6, 2015.
-
Qi XP, Zhao JQ, Du ZF, et al.: Prophylactic thyroidectomy for MEN 2-related medullary thyroid carcinoma based on predictive testing for RET proto-oncogene mutation and basal serum calcitonin in China. Eur J Surg Oncol 39 (9): 1007-12, 2013.
-
Gagel RF, Tashjian AH Jr, Cummings T, et al.: The clinical outcome of prospective screening for multiple endocrine neoplasia type 2a. An 18-year experience. N Engl J Med 318 (8): 478-84, 1988.
-
Schreinemakers JM, Vriens MR, Valk GD, et al.: Factors predicting outcome of total thyroidectomy in young patients with multiple endocrine neoplasia type 2: a nationwide long-term follow-up study. World J Surg 34 (4): 852-60, 2010.
-
Niccoli-Sire P, Murat A, Baudin E, et al.: Early or prophylactic thyroidectomy in MEN 2/FMTC gene carriers: results in 71 thyroidectomized patients. The French Calcitonin Tumours Study Group (GETC). Eur J Endocrinol 141 (5): 468-74, 1999.
-
Wells SA Jr, Skinner MA: Prophylactic thyroidectomy, based on direct genetic testing, in patients at risk for the multiple endocrine neoplasia type 2 syndromes. Exp Clin Endocrinol Diabetes 106 (1): 29-34, 1998.
-
Szinnai G, Meier C, Komminoth P, et al.: Review of multiple endocrine neoplasia type 2A in children: therapeutic results of early thyroidectomy and prognostic value of codon analysis. Pediatrics 111 (2): E132-9, 2003.
-
Skinner MA, Moley JA, Dilley WG, et al.: Prophylactic thyroidectomy in multiple endocrine neoplasia type 2A. N Engl J Med 353 (11): 1105-13, 2005.
-
Machens A, Schneyer U, Holzhausen HJ, et al.: Prospects of remission in medullary thyroid carcinoma according to basal calcitonin level. J Clin Endocrinol Metab 90 (4): 2029-34, 2005.
-
Machens A, Lorenz K, Dralle H: Individualization of lymph node dissection in RET (rearranged during transfection) carriers at risk for medullary thyroid cancer: value of pretherapeutic calcitonin levels. Ann Surg 250 (2): 305-10, 2009.
-
Franc S, Niccoli-Sire P, Cohen R, et al.: Complete surgical lymph node resection does not prevent authentic recurrences of medullary thyroid carcinoma. Clin Endocrinol (Oxf) 55 (3): 403-9, 2001.
-
van Heurn LW, Schaap C, Sie G, et al.: Predictive DNA testing for multiple endocrine neoplasia 2: a therapeutic challenge of prophylactic thyroidectomy in very young children. J Pediatr Surg 34 (4): 568-71, 1999.
-
Hansen HS, Torring H, Godballe C, et al.: Is thyroidectomy necessary in RET mutations carriers of the familial medullary thyroid carcinoma syndrome? Cancer 89 (4): 863-7, 2000.
-
Mandel SJ, Brent GA, Larsen PR: Levothyroxine therapy in patients with thyroid disease. Ann Intern Med 119 (6): 492-502, 1993.
-
Sawin CT, Geller A, Hershman JM, et al.: The aging thyroid. The use of thyroid hormone in older persons. JAMA 261 (18): 2653-5, 1989.
-
Baloch Z, Carayon P, Conte-Devolx B, et al.: Laboratory medicine practice guidelines. Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 13 (1): 3-126, 2003.
-
Seib CD, Harari A, Conte FA, et al.: Utility of serum thyroglobulin measurements after prophylactic thyroidectomy in patients with hereditary medullary thyroid cancer. Surgery 156 (2): 394-8, 2014.
-
Samaan NA, Schultz PN, Hickey RC: Medullary thyroid carcinoma: prognosis of familial versus nonfamilial disease and the role of radiotherapy. Horm Metab Res Suppl 21: 21-5, 1989.
-
Scherübl H, Raue F, Ziegler R: Combination chemotherapy of advanced medullary and differentiated thyroid cancer. Phase II study. J Cancer Res Clin Oncol 116 (1): 21-3, 1990.
-
Cohen EE, Rosen LS, Vokes EE, et al.: Axitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: results from a phase II study. J Clin Oncol 26 (29): 4708-13, 2008.
-
Lam ET, Ringel MD, Kloos RT, et al.: Phase II clinical trial of sorafenib in metastatic medullary thyroid cancer. J Clin Oncol 28 (14): 2323-30, 2010.
-
Carr LL, Mankoff DA, Goulart BH, et al.: Phase II study of daily sunitinib in FDG-PET-positive, iodine-refractory differentiated thyroid cancer and metastatic medullary carcinoma of the thyroid with functional imaging correlation. Clin Cancer Res 16 (21): 5260-8, 2010.
-
Kurzrock R, Sherman SI, Ball DW, et al.: Activity of XL184 (Cabozantinib), an oral tyrosine kinase inhibitor, in patients with medullary thyroid cancer. J Clin Oncol 29 (19): 2660-6, 2011.
-
Wells SA Jr, Robinson BG, Gagel RF, et al.: Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol 30 (2): 134-41, 2012.
-
Fox E, Widemann BC, Chuk MK, et al.: Vandetanib in children and adolescents with multiple endocrine neoplasia type 2B associated medullary thyroid carcinoma. Clin Cancer Res 19 (15): 4239-48, 2013.
-
Elisei R, Schlumberger MJ, Müller SP, et al.: Cabozantinib in progressive medullary thyroid cancer. J Clin Oncol 31 (29): 3639-46, 2013.
-
Castinetti F, Qi XP, Walz MK, et al.: Outcomes of adrenal-sparing surgery or total adrenalectomy in phaeochromocytoma associated with multiple endocrine neoplasia type 2: an international retrospective population-based study. Lancet Oncol 15 (6): 648-55, 2014.
-
Thosani S, Ayala-Ramirez M, Palmer L, et al.: The characterization of pheochromocytoma and its impact on overall survival in multiple endocrine neoplasia type 2. J Clin Endocrinol Metab 98 (11): E1813-9, 2013.
-
Lairmore TC, Ball DW, Baylin SB, et al.: Management of pheochromocytomas in patients with multiple endocrine neoplasia type 2 syndromes. Ann Surg 217 (6): 595-601; discussion 601-3, 1993.
-
Okamoto T, Obara T, Ito Y, et al.: Bilateral adrenalectomy with autotransplantation of adrenocortical tissue or unilateral adrenalectomy: treatment options for pheochromocytomas in multiple endocrine neoplasia type 2A. Endocr J 43 (2): 169-75, 1996.
-
Inabnet WB, Caragliano P, Pertsemlidis D: Pheochromocytoma: inherited associations, bilaterality, and cortex preservation. Surgery 128 (6): 1007-11;discussion 1011-2, 2000.
-
Scholten A, Valk GD, Ulfman D, et al.: Unilateral subtotal adrenalectomy for pheochromocytoma in multiple endocrine neoplasia type 2 patients: a feasible surgical strategy. Ann Surg 254 (6): 1022-7, 2011.
-
Grubbs EG, Rich TA, Ng C, et al.: Long-term outcomes of surgical treatment for hereditary pheochromocytoma. J Am Coll Surg 216 (2): 280-9, 2013.
-
Walz MK, Alesina PF, Wenger FA, et al.: Posterior retroperitoneoscopic adrenalectomy--results of 560 procedures in 520 patients. Surgery 140 (6): 943-8; discussion 948-50, 2006.
-
Walz MK, Alesina PF, Wenger FA, et al.: Laparoscopic and retroperitoneoscopic treatment of pheochromocytomas and retroperitoneal paragangliomas: results of 161 tumors in 126 patients. World J Surg 30 (5): 899-908, 2006.
-
Perrier ND, Kennamer DL, Bao R, et al.: Posterior retroperitoneoscopic adrenalectomy: preferred technique for removal of benign tumors and isolated metastases. Ann Surg 248 (4): 666-74, 2008.
-
Behrman SW, Bahr MH, Dickson PV, et al.: The microbiology of secondary and postoperative pancreatic infections: implications for antimicrobial management. Arch Surg 146 (5): 613-9, 2011.
-
Evans DB, Perrier ND: On "Posterior retroperitoneoscopic adrenalectomy--results of 560 procedures in 520 patients". Surgery 140 (6): 951-2, 2006.
-
Dickson PV, Jimenez C, Chisholm GB, et al.: Posterior retroperitoneoscopic adrenalectomy: a contemporary American experience. J Am Coll Surg 212 (4): 659-65; discussion 665-7, 2011.
-
Norton JA, Brennan MF, Wells SA Jr: Surgical Management of Hyperparathyroidism. In: Bilezikian JP, Marcus R, Levine MA: The Parathyroids: Basic and Clinical Concepts. New York: Raven Press, 1994, pp 531-551.
-
Khan MI, Waguespack SG, Hu MI: Medical management of postsurgical hypoparathyroidism. Endocr Pract 17 (Suppl 1): 18-25, 2011 Mar-Apr.
-
Stålberg P, Carling T: Familial parathyroid tumors: diagnosis and management. World J Surg 33 (11): 2234-43, 2009.
-
Peacock M, Bilezikian JP, Klassen PS, et al.: Cinacalcet hydrochloride maintains long-term normocalcemia in patients with primary hyperparathyroidism. J Clin Endocrinol Metab 90 (1): 135-41, 2005.
-
Schuffenecker I, Ginet N, Goldgar D, et al.: Prevalence and parental origin of de novo RET mutations in multiple endocrine neoplasia type 2A and familial medullary thyroid carcinoma. Le Groupe d'Etude des Tumeurs a Calcitonine. Am J Hum Genet 60 (1): 233-7, 1997.
-
Norum RA, Lafreniere RG, O'Neal LW, et al.: Linkage of the multiple endocrine neoplasia type 2B gene (MEN2B) to chromosome 10 markers linked to MEN2A. Genomics 8 (2): 313-7, 1990.
-
Carlson KM, Bracamontes J, Jackson CE, et al.: Parent-of-origin effects in multiple endocrine neoplasia type 2B. Am J Hum Genet 55 (6): 1076-82, 1994.
-
Kitamura Y, Scavarda N, Wells SA Jr, et al.: Two maternally derived missense mutations in the tyrosine kinase domain of the RET protooncogene in a patient with de novo MEN 2B. Hum Mol Genet 4 (10): 1987-8, 1995.
-
Rich TA, Liu M, Etzel CJ, et al.: Comparison of attitudes regarding preimplantation genetic diagnosis among patients with hereditary cancer syndromes. Fam Cancer 13 (2): 291-9, 2014.
-
Freyer G, Ligneau B, Schlumberger M, et al.: Quality of life in patients at risk of medullary thyroid carcinoma and followed by a comprehensive medical network: trends for future evaluations. Ann Oncol 12 (10): 1461-5, 2001.
-
Freyer G, Dazord A, Schlumberger M, et al.: Psychosocial impact of genetic testing in familial medullary-thyroid carcinoma: a multicentric pilot-evaluation. Ann Oncol 10 (1): 87-95, 1999.
-
Grosfeld FJ, Lips CJ, Ten Kroode HF, et al.: Psychosocial consequences of DNA analysis for MEN type 2. Oncology (Huntingt) 10 (2): 141-6; discussion 146, 152, 157, 1996.
-
Johnston LB, Chew SL, Trainer PJ, et al.: Screening children at risk of developing inherited endocrine neoplasia syndromes. Clin Endocrinol (Oxf) 52 (2): 127-36, 2000.
-
MacDonald DJ, Lessick M: Hereditary cancers in children and ethical and psychosocial implications. J Pediatr Nurs 15 (4): 217-25, 2000.
-
Grosfeld FJ, Lips CJ, Beemer FA, et al.: Psychological risks of genetically testing children for a hereditary cancer syndrome. Patient Educ Couns 32 (1-2): 63-7, 1997 Sep-Oct.
-
Giarelli E: Multiple endocrine neoplasia type 2a (MEN2a): a call for psycho-social research. Psychooncology 11 (1): 59-73, 2002 Jan-Feb.
-
Grosfeld FJ, Lips CJ, Beemer FA, et al.: Distress in MEN 2 family members and partners prior to DNA test disclosure. Multiple endocrine neoplasia type 2. Am J Med Genet 91 (1): 1-7, 2000.
-
Grosfeld FJ, Beemer FA, Lips CJ, et al.: Parents' responses to disclosure of genetic test results of their children. Am J Med Genet 94 (4): 316-23, 2000.
-
Giarelli E: Bringing threat to the fore: participating in lifelong surveillance for genetic risk of cancer. Oncol Nurs Forum 30 (6): 945-55, 2003 Nov-Dec.
-
Schultz PN: Providing information to patients with a rare cancer: using Internet discussion forums to address the needs of patients with medullary thyroid carcinoma. Clin J Oncol Nurs 6 (4): 219-22, 2002 Jul-Aug.
Familial Pheochromocytoma and Paraganglioma SyndromeIntroduction Paragangliomas (PGLs) and pheochromocytomas (PHEOs) are rare tumors arising from chromaffin cells, which have the ability to synthesize, store, and secrete catecholamines and neuropeptides. Individuals may present with secondary hypertension. In 2004, the World Health Organization characterized adrenal gland tumors as PHEOs.[1] The term paraganglioma is reserved for non-adrenal (or extra-adrenal) neoplasms and may arise in various sites from the paraganglia along the parasympathetic nerves or the sympathetic trunk. PGLs may be found in the head and neck region, abdomen, or pelvis. Only those arising from sympathetic neural chains have secretory capacity. PGLs found in the skull base or head and neck region typically arise in the glomus cells, near the carotid body, along the vagal nerve or jugular fosse, and are usually from parasympathetic paraganglia and therefore rarely secrete catecholamines.[2,3] The most recognizable tumors are found at the carotid body. PGLs below the neck are most commonly located in the upper mediastinum or the urinary bladder.[3] The reported incidence of these tumors in the general population is variable because they may be asymptomatic but ranges from 1 in 30,000 to 1 in 100,000 individuals.[3] One autopsy study found a much greater incidence of 1 in 2,000 individuals, suggesting a high frequency of occult tumors.[4] PGLs have an equal sex distribution and can occur at any age but have the highest incidence between the ages of 40 and 50 years.[5,6] Clinical Description PGLs and PHEOs may occur sporadically, as a manifestation of a hereditary syndrome, or as the sole tumor in one of several hereditary PGL/PHEO syndromes. PGLs and PHEOs are typically slow-growing tumors, and some may be present for many years before coming to clinical attention. Conversely, a minority of these tumors may be malignant and present with a more aggressive clinical course. PGL and PHEO malignancy is defined by the presence of metastases at sites distant from the primary tumor in nonchromaffin tissue. Common sites of metastases include bone, liver, and lungs.[1] There are no reliable molecular, immunohistochemical, or genetic predictors to distinguish benign and malignant tumors,[7] although some studies have shown a higher malignancy rate in SDHBcarriers [8] and in individuals with larger tumors.[9] Some experts view local invasion into surrounding tissue as an additional marker of malignancy.[10,11] Others have disagreed with this classification because locally invasive tumors tend to follow a more indolent course than tumors with distant metastatic involvement.[12] Consequently, estimation of the rate of malignancy in PGLs is difficult; rates ranging from 5% to 20% have been reported.[13,14,15] Clinical Diagnosis of PGL and PHEO A PGL may cause a variety of symptoms depending on the location of the tumor and whether the tumor has secretory capacity. PGLs of the head and neck are rarely associated with elevated catecholamines. Secretory PGLs and PHEOs may cause hypertension, headache, tachycardia, sweating, and flushing. Typically, nonsecretory tumors are painless, coming to attention only when growth of the lesion into surrounding structures causes a mass effect. Patients with a head or neck PGL may present with an enlarging lateral neck mass, hoarseness, Horner syndrome, pulsatile tinnitus, dizziness, facial droop, or blurred vision.[1] Patients with clinically apparent catecholamine excess generally undergo biochemical testing to evaluate the secretory capacity of the tumor(s).[16] This evaluation is best performed by measuring urine and/or plasma fractionated metanephrines (normetanephrine and metanephrine), which yields a higher sensitivity and specificity than directly measuring catecholamines (norepinephrine, dopamine, and epinephrine).[17,18,19] For patients whose plasma metanephrines levels are measured, blood is collected after an intravenous catheter has been inserted and the patient has been in a supine position for 15 to 20 minutes.[20] Additionally, the patient should not have food or caffeinated beverages, smoke cigarettes, or engage in strenuous physical activity in the 8 to 12 hours before the blood draw.[20] Imaging of PGLs is the mainstay of diagnosis; the initial evaluation includes computed tomography (CT) of the neck and chest. Magnetic resonance imaging (MRI) also has utility for the head and neck. PGLs typically appear homogeneous with intense enhancement after administration of intravenous contrast. MRI may also be used to distinguish the tumor from adjacent vascular and skeletal structures. On T2-weighted images, a tumor that is larger than 2 cm is likely to display a classic "salt and pepper" appearance, a reflection of scattered areas of signal void mingled with areas of high signal intensity from increased vascularity.[21] Nuclear imaging, particularly somatostatin receptor scintigraphy (SRS) in combination with anatomic imaging, may be useful for localization and determination of the extent of disease (multifocality vs. distant metastatic deposits).[22] Benign tumors are reported to be more sensitive to SRS than iodine I 123-metaiodobenzylguanidine (123I-MIBG) imaging. Sensitivity is highest for the head and neck region compared with abdomen PGLs or PHEOs (91% vs. 40% and 42%, respectively).[23] SRS has been reported to be superior to MIBG in detecting metastatic tumors (95% vs. 23%, respectively).[23] 123I-MIBG, however, is highly sensitive for PHEO [23] and positron emission tomography-computed tomography (PET-CT) is very specific for PGLs. Functional imaging for PGLs and/or PHEOs with fluorine F 18-dihydroxyphenylalanine (18F-DOPA), 18F-fluorodopamine, or PET-CT may be particularly helpful in localizing head and neck tumors. Data suggest that the selection of PET tracer utilized for tumor localization should be centered on the patient's genetic status, based on the metabolic activity of the various tumors.[8] It has been suggested that patients with SDHx and VHLpathogenic variants are more likely to have higher 18F-fluorodeoxyglucose activity, which is related to gene activation in response to hypoxia.[8,24] Some SDHB tumors only weakly concentrate 18F-DOPA, and patients with SDHx pathogenic variants may have false-negative results with such scans. Gallium Ga 68-DOTATATE PET-CT shows promise as a potential imaging modality for determining the extent of disease in patients with metastatic involvement.[25] Tumors with VHL pathogenic variants may likewise be missed with MIBG scans.[8] Imaging of PHEOs usually consists of a dedicated CT of the adrenal gland. When biochemical screening in an individual who has or is at risk of multiple endocrine neoplasia type 2 (MEN2) suggests PHEO, localization studies, such as MRI or CT, can be performed.[26] Confirmation of the diagnosis can be made using iodine I 131-MIBG scintigraphy or PET imaging.[26,27,28,29] Genetics, Inheritance, and Genetic Testing A significant proportion of individuals presenting with apparently sporadic PHEO or PGL are carriers of germline pathogenic variants. Up to 33% of patients with apparently sporadic PHEO, and up to 40% of patients with apparently sporadic PGLs, actually have a recognizable germline pathogenic variant in one of the known PGL/PHEO susceptibility genes.[14,30,31,32,33,34] One study found that in individuals with a single tumor and a negative family history, the likelihood of an inherited pathogenic variant was 11.6%,[14] whereas other groups detected pathogenic variants in 41% of such patients.[34,35] For example, even among carriers of SDHB pathogenic variants, there is low penetrance and delayed onset of disease, which may further obscure the hereditary nature of the disease.[36] As such, all patients with PHEO or PGL, even those with apparently sporadic tumors, may be considered for genetic testing because of the high frequency of pathogenic variants associated with these conditions.[37] PGLs and PHEOs can be seen as part of several well-described tumor susceptibility syndromes including von Hippel-Lindau (VHL), MEN2, neurofibromatosis type 1, Carney-Stratakis syndrome, and familial paraganglioma (FPGL) syndrome. FPGL is most commonly caused by pathogenic variants in one of the following four genes: SDHA, SDHB, SDHC, and SDHD (collectively referred to as SDHx). The SDHx proteins form part of the succinate dehydrogenase (SDH) complex, which is located on the inner mitochondrial membrane and plays a critical role in cellular energy metabolism.[38] Pathogenic variants in SDHB are most common, followed by SDHD and rarely SDHC and SDHA. More recently, pathogenic variants in the SDHAF2 (also called SDH5), TMEM127, and MAX genes have been described in FPGL/PHEO,[39,40,41,42] but these variants are rare. The mechanism of tumor formation has remained elusive. One study suggests that SDHx-associated tumors display a hypermethylator phenotype that is associated with downregulation of important genes involved in the differentiation of neuroendocrine tissues.[43] The inheritance pattern of FPGL depends on the gene involved. While most families show traditional autosomal dominant inheritance, those with pathogenic variants in SDHAF2 and SDHD show almost exclusive paternal transmission of the phenotype. In other words, while the pathogenic variant can be passed down from mother or father, tumors will develop only if the pathogenic variant is inherited from the father.[44,45] In cases of FPGL not caused by SDHD or SDHAF2 pathogenic variants, first-degree relatives (FDRs) of an affected individual have a 50% chance of carrying the pathogenic variant and are at increased risk of developing PGLs. Because the family history can appear negative in families with lower penetrance pathogenic variants, it is important to offer genetic testing to all unaffected FDRs once the pathogenic variant in the family has been identified. Genetic testing for hereditary PHEO and PGL syndromes is largely based on published algorithms,[37] whereby testing is performed stepwise based on factors such as tumor type and location, age at diagnosis, family history, and presence of malignancy.[14,46,47] This approach has allowed for cost-effective, targeted testing based on clinical features. Within the last several years, however, next-generation sequencing (NGS) technology has led to a dramatic decrease in the cost of genetic testing, and testing for pathogenic variants in 10 to 30 genes for the same cost of testing two or three genes is now possible. These tests may be more appropriate for individuals and families who have an atypical presentation or overlapping clinical features. If the cost associated with multigene testing panels continues to decrease, the testing algorithms may soon be obsolete for PGL and PHEO. A recent series analyzed 85 PGL and PHEO samples using an NGS panel test for the ten known PGL susceptibility genes and showed a sensitivity of 98.7%.[48] Genotype-Phenotype Correlations In FPGL/PHEO, the type and location of tumors, age at onset, and lifetime penetrance vary depending on the genetic variant. While these correlations can help guide genetic testing and screening decisions, caution must be used given the high degree of variability seen in this condition. FPGL/PHEO syndromes are among the rare inherited diseases in which genomic imprinting occurs. For example, the SDHD pathogenic variant is normally not activated when inherited from the mother, and the risk of FPGL/PHEO syndromes is not increased. However, the pathogenic variant is turned on when the gene is inherited from the father, and the risk is increased. SDHD pathogenic variants are mainly associated with an increased risk of parasympathetic PGLs. These are more commonly multifocal and located in the head and neck, while tumors in SDHB carriers are more often located in the abdomen.[49,50] One series showed a risk of 71% for a head and neck tumor in SDHD carriers, as opposed to a 29% risk in SDHB carriers. The lifetime risk for any PGL in any location in SDHD carriers was estimated to be as high as 77% by age 50 years in one series [49] and 90% by age 70 years in a second series.[50] A review of more than 1,700 cases reported in the literature provided similar estimates, suggesting a lifetime penetrance of 86%.[51] The rate of malignancy in SDHD carriers is lower than 5%.[51] Pathogenic variants in the SDHB gene are associated with sympathetic PGLs, although PHEO and parasympathetic PGLs also have been described. SDHB PGLs are more commonly located in the abdomen and mediastinum than in the head and neck. A review of 1,700 cases suggested a lifetime penetrance of 77%.[51] However, many early studies examining penetrance were subject to ascertainment bias due to sampling of highly suggestive individuals affected at young ages, with limited inclusion of asymptomatic pathogenic variant carriers. More recent family-based studies have found lower penetrance estimates, ranging from 9% to 35% by age 50 years.[36,52,53,54] The rate of malignancy is higher with SDHB than with the other SDH genes, with up to one-third of patients having malignant tumors in most series.[49,50] Pathogenic variants in SDHB have also been associated with several other tumors and malignancies, including gastrointestinal stromal tumors (GISTs), renal cell carcinoma, and papillary thyroid cancer.[49,50] SDHC pathogenic variants are rare, accounting for an estimated 0.5% of all PGLs.[51] In one series of 153 patients with multiple PGLs or a single PGL diagnosed before age 40 years, three (2%) had an SDHC pathogenic variant.[31] Another series of 121 index cases from a head and neck PGL registry showed a pathogenic variant rate of 4% (5 of 121).[55]SDHC pathogenic variants most commonly cause head and neck PGLs but have been seen in a small number of patients with abdominal PGLs.[14,56] Pathogenic variants in SDHB, SDHC, and SDHD can also cause Carney-Stratakis syndrome, which is characterized by the dyad of PGLs and GISTs.[57] Pathogenic variants in SDHA, SDAHF2, MAX, and TMEM127 have been described in a small number of cases. Collectively, they account for less than 2% to 3% of all cases. Although biallelic pathogenic variants in SDHA have long been known to cause the autosomal recessive condition inherited juvenile encephalopathy/Leigh syndrome,[58] it was not until recently that monoallelic pathogenic variants were linked to an increased risk of developing PGL. Only a handful of cases have been described. Tumors can develop in the head and neck, the adrenal glands, or in the abdomen (extra-adrenal).[59,60] The SDHAF2 gene encodes a protein that is responsible for flavination of SDHA and proper functioning of the SDHA subunit of the SDH complex. To date, pathogenic variants in SDHAF2 have been described in fewer than 20 cases and only with head and neck PGLs.[42] The MAX gene was first described as a PHEO susceptibility gene in 2011 through exome sequencing of three unrelated cases.[39] Three different germline pathogenic variants were identified, and a follow-up series of 59 cases by the same group identified an additional five variants. The MAX protein is part of MYC-MAX-MXD1 network, which plays a key role in the development and progression of neural crest cell tumors.[61] The TMEM127 gene is located on chromosome 2q11.2 and encodes a transmembrane protein known to be a negative regulator of mTOR, which regulates multiple cellular processes. A review of 23 patients with TMEM127 pathogenic variants showed that 96% (22 of 23) had a PHEO and 9% (2 of 23) had a PGL.[51] Surveillance Patients with an identified germline pathogenic variant in one of the SDH genes are at a significantly increased risk of developing PGLs, PHEOs, renal tumors, and GISTs. PHEOs and PGLs typically have a slow growth pattern, but unchecked growth can lead to mass effect and, ultimately, neurologic compromise. Further, although most of these tumors are benign, some may undergo malignant transformation. As such, periodic screening for interval development of a tumor is of critical importance because early detection and removal can minimize risk to the patient. Although limited studies have been performed to delineate the ideal protocol, total-body MRI has been proposed as a reasonable method for screening because of its high sensitivity and minimal radiation exposure.[37,62] In one study, 37 carriers of SDHx pathogenic variants underwent annual biochemical testing and annual or biennial whole-body MRI beginning at age 10 years.[63] This screening protocol identified six tumors in five patients. The sensitivity of MRI was 87.5%, and the specificity was 94.7%. The sensitivity of biochemical testing was significantly lower at 37.5%, with a specificity similar to MRI at 94.9%.[63] A more-recent retrospective study of 157 patients evaluated a rapid contrast-enhanced angio-MRI protocol for the detection of head and neck paragangliomas in carriers of SDH pathogenic variants.[64] This protocol had a high sensitivity and specificity of 88.7% and 93.7%, respectively. Although the optimal imaging protocol for surveillance in carriers of SDH pathogenic variants remains unclear, annual biochemical testing and clinical surveillance may be considered. Biochemical testing can be performed by measuring plasma-free metanephrines/catecholamines or 24-hour urinary excretion of fractionated catecholamines (including methoxytyramine, a dopamine metabolite, if available). Clinical surveillance may include physical examination and blood pressure measurement. Clinical surveillance and biochemical testing may begin between ages 5 years and 10 years, or 10 years earlier than the earliest age at diagnosis in the family.[65,66] Level of evidence: 4 Interventions Preoperative management Medical management is the bridge to surgical resection of PGLs/PHEOs. Preoperative medical therapy is not essential for patients without evidence of catecholamine hypersecretion, although some advocate its use regardless of the results of hormonal testing.[20] The aim of pharmacologic therapy is to control hypertension for at least 10 to 14 days before surgery.[67] Management is aimed at preventing catecholamine-induced complications, even in patients who may not present with preoperative hypertension, to avoid intraoperative hypertensive crisis, cardiac arrhythmias, pulmonary edema, and cardiac ischemia. Failure to adequately block the catecholamine excess can dramatically increase the risk of perioperative mortality from hypertensive crisis and lethal arrhythmias and cause hypotensive crisis after tumor removal.[68,69] In the absence of a randomized controlled trial comparing the various regimens, there is no universally recommended approach. The alpha-adrenoreceptor blocker phenoxybenzamine (Dibenzyline) is most frequently used to control blood pressure and expand the blood volume.[20] Other alpha-blocking drugs have also been used with success, including prazosin, terazosin, or doxazosin; these drugs are more specific alpha-1 adrenergic competitive antagonists and have a shorter half-life than phenoxybenzamine.[70,71] The noncompetitive binding of phenoxybenzamine to the alpha receptors, coupled with its longer half-life, may result in a sustained effect of the drug, with some patients experiencing postoperative hypotension.[20,72] One study found that patients treated with sustained-release doxazosin had more stable perioperative hemodynamic changes and a shorter time interval to preoperative blood pressure control than did patients who received phenoxybenzamine.[72] Once the alpha blockade is initiated, expansion of the blood volume is often necessary, as these patients are typically volume contracted.[73,74] In addition to the vasodilatory effects from alpha blockade, volume expansion may be achieved by consuming a high-sodium diet and high fluid intake or a preoperative saline infusion. A clinical manifestation of adequate blockade is the symptom of nasal stuffiness or lightheadedness. Calcium channel blockers such as nicardipine or nifedipine also have been employed to control the hypertension preoperatively.[75] A calcium channel blocker may be used in conjunction with alpha and beta blockade for refractory hypertension or used alone as a second-line agent for patients with intolerable side effects from alpha blockade.[20] Surgery Surgical resection is the treatment of choice for PGL and PHEO. Both open resection and laparoscopic approaches are safe, but if feasible, laparoscopic removal is preferred.[65,76] Open resection is commonly recommended for large tumors (>6 cm-7 cm) because of the increased risk of technical difficulty within the confined space of laparoscopy. Means of exposure and approach are based on the anatomic location of the tumor. Direct access to the adrenal and para-aortic region can be achieved with the posterior approach. It is direct, safe, and efficient.[77] Adequate exposure of the complete tumor is important for complete removal. Robotic assistance can be utilized in select cases because it offers a three-dimensional, magnified view of the anatomy.[78] The efficacy and safety of posterior retroperitoneoscopic adrenalectomy is established, but ongoing studies are examining the relevance of this approach in familial syndromes (see NCT02618694). PGLs are commonly located in the para-aortic retroperitoneal sympathetic chain above the aortic bifurcation, below the takeoff of the inferior mesenteric artery (organ of Zuckerkandl), or near the dome of the bladder.[79,80] Malignant PGLs have a dense fibrous capsule that may be adherent to surrounding vascularity, which can make complete resection difficult.[80] Regional lymph nodes may be involved with malignant tumors, and if suspected preoperatively or noted intraoperatively, a regional lymphadenectomy may be performed. Genetic testing is best performed before the initial surgery to inform the risk of recurrent or contralateral disease and to guide the extent of resection (e.g., whether to preserve the cortex) because synchronous or metachronous bilateral disease is quite common in hereditary PHEO. In one retrospective series that spanned nearly 50 years, 15 of the 49 patients (30%) who presented with a unilateral PHEO and underwent unilateral total adrenalectomy developed PHEO in the contralateral gland at a median of 8.2 years (range, 1-20 years) after initial diagnosis.[81] Of the 15 patients who developed PHEO in the contralateral gland, 8 had MEN2A, 2 had MEN2B, 2 had VHL, and 1 had familial PHEO. The risk of developing a contralateral tumor increased over time, with 25% of patients developing tumors after a median of 6 years and 43% after a median of 32 years. Cortical-sparing surgery is an attractive option because it minimizes the risk of adrenal insufficiency and the need for lifelong steroid supplementation. In large series of patients, cortical-sparing surgery has a 3% to 7% recurrence rate after cortical preservation versus a 2% to 3% recurrence rate after total resection (recurrence in the adrenal bed).[81,82] The frequency of steroid dependence in both studies was lower in patients who underwent cortical-sparing techniques than in patients who did not (57% compared to 86%). One of 39 patients (3%) developed adrenal insufficiency after a cortical-sparing procedure; 5 of 25 patients (20%) developed adrenal insufficiency after total adrenalectomy.[81] These study authors recommend cortical-sparing surgery as a viable option for patients with hereditary PHEO, including patients who initially present with seemingly unilateral disease. Level of evidence: 5 References:
-
DeLellis RA, Lloyd RV, Heitz PU, et al., eds.: Pathology and Genetics of Tumours of Endocrine Organs. Lyon, France: IARC Press, 2004. World Health Organization classification of tumours, vol. 8.
-
Offergeld C, Brase C, Yaremchuk S, et al.: Head and neck paragangliomas: clinical and molecular genetic classification. Clinics (Sao Paulo) 67 (Suppl 1): 19-28, 2012.
-
Raygada M, Pasini B, Stratakis CA: Hereditary paragangliomas. Adv Otorhinolaryngol 70: 99-106, 2011.
-
McNeil AR, Blok BH, Koelmeyer TD, et al.: Phaeochromocytomas discovered during coronial autopsies in Sydney, Melbourne and Auckland. Aust N Z J Med 30 (6): 648-52, 2000.
-
O'Riordain DS, Young WF Jr, Grant CS, et al.: Clinical spectrum and outcome of functional extraadrenal paraganglioma. World J Surg 20 (7): 916-21; discussion 922, 1996.
-
Erickson D, Kudva YC, Ebersold MJ, et al.: Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. J Clin Endocrinol Metab 86 (11): 5210-6, 2001.
-
Jovanovic R, Kostadinova-Kunovska S, Bogoeva B, et al.: Histological features, Ki-67 and Bcl-2 immunohistochemical expression and their correlation with the aggressiveness of pheochromocytomas. Prilozi 33 (2): 23-40, 2012.
-
Taïeb D, Neumann H, Rubello D, et al.: Modern nuclear imaging for paragangliomas: beyond SPECT. J Nucl Med 53 (2): 264-74, 2012.
-
Eisenhofer G, Lenders JW, Siegert G, et al.: Plasma methoxytyramine: a novel biomarker of metastatic pheochromocytoma and paraganglioma in relation to established risk factors of tumour size, location and SDHB mutation status. Eur J Cancer 48 (11): 1739-49, 2012.
-
Eisenhofer G, Bornstein SR, Brouwers FM, et al.: Malignant pheochromocytoma: current status and initiatives for future progress. Endocr Relat Cancer 11 (3): 423-36, 2004.
-
Zarnegar R, Kebebew E, Duh QY, et al.: Malignant pheochromocytoma. Surg Oncol Clin N Am 15 (3): 555-71, 2006.
-
Medeiros LJ, Wolf BC, Balogh K, et al.: Adrenal pheochromocytoma: a clinicopathologic review of 60 cases. Hum Pathol 16 (6): 580-9, 1985.
-
Walz MK, Alesina PF, Wenger FA, et al.: Laparoscopic and retroperitoneoscopic treatment of pheochromocytomas and retroperitoneal paragangliomas: results of 161 tumors in 126 patients. World J Surg 30 (5): 899-908, 2006.
-
Mannelli M, Castellano M, Schiavi F, et al.: Clinically guided genetic screening in a large cohort of italian patients with pheochromocytomas and/or functional or nonfunctional paragangliomas. J Clin Endocrinol Metab 94 (5): 1541-7, 2009.
-
Lee JH, Barich F, Karnell LH, et al.: National Cancer Data Base report on malignant paragangliomas of the head and neck. Cancer 94 (3): 730-7, 2002.
-
Grossman A, Pacak K, Sawka A, et al.: Biochemical diagnosis and localization of pheochromocytoma: can we reach a consensus? Ann N Y Acad Sci 1073: 332-47, 2006.
-
Lenders JW, Pacak K, Walther MM, et al.: Biochemical diagnosis of pheochromocytoma: which test is best? JAMA 287 (11): 1427-34, 2002.
-
Eisenhofer G, Lenders JW, Linehan WM, et al.: Plasma normetanephrine and metanephrine for detecting pheochromocytoma in von Hippel-Lindau disease and multiple endocrine neoplasia type 2. N Engl J Med 340 (24): 1872-9, 1999.
-
Sawka AM, Jaeschke R, Singh RJ, et al.: A comparison of biochemical tests for pheochromocytoma: measurement of fractionated plasma metanephrines compared with the combination of 24-hour urinary metanephrines and catecholamines. J Clin Endocrinol Metab 88 (2): 553-8, 2003.
-
Chen H, Sippel RS, O'Dorisio MS, et al.: The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas 39 (6): 775-83, 2010.
-
Olsen WL, Dillon WP, Kelly WM, et al.: MR imaging of paragangliomas. AJR Am J Roentgenol 148 (1): 201-4, 1987.
-
Gimenez-Roqueplo AP, Dahia PL, Robledo M: An update on the genetics of paraganglioma, pheochromocytoma, and associated hereditary syndromes. Horm Metab Res 44 (5): 328-33, 2012.
-
Michałowska I, Ćwikła JB, Pęczkowska M, et al.: Usefulness of Somatostatin Receptor Scintigraphy (Tc-[HYNIC, Tyr3]-Octreotide) and 123I-Metaiodobenzylguanidine Scintigraphy in Patients with SDHx Gene-Related Pheochromocytomas and Paragangliomas Detected by Computed Tomography. Neuroendocrinology 101 (4): 321-30, 2015.
-
Span PN, Rao JU, Oude Ophuis SB, et al.: Overexpression of the natural antisense hypoxia-inducible factor-1alpha transcript is associated with malignant pheochromocytoma/paraganglioma. Endocr Relat Cancer 18 (3): 323-31, 2011.
-
Janssen I, Blanchet EM, Adams K, et al.: Superiority of [68Ga]-DOTATATE PET/CT to Other Functional Imaging Modalities in the Localization of SDHB-Associated Metastatic Pheochromocytoma and Paraganglioma. Clin Cancer Res 21 (17): 3888-95, 2015.
-
Pacak K, Eisenhofer G, Ahlman H, et al.: Pheochromocytoma: recommendations for clinical practice from the First International Symposium. October 2005. Nat Clin Pract Endocrinol Metab 3 (2): 92-102, 2007.
-
Lips CJ, Landsvater RM, Höppener JW, et al.: Clinical screening as compared with DNA analysis in families with multiple endocrine neoplasia type 2A. N Engl J Med 331 (13): 828-35, 1994.
-
van der Harst E, de Herder WW, Bruining HA, et al.: [(123)I]metaiodobenzylguanidine and [(111)In]octreotide uptake in begnign and malignant pheochromocytomas. J Clin Endocrinol Metab 86 (2): 685-93, 2001.
-
Pacak K, Linehan WM, Eisenhofer G, et al.: Recent advances in genetics, diagnosis, localization, and treatment of pheochromocytoma. Ann Intern Med 134 (4): 315-29, 2001.
-
Jafri M, Whitworth J, Rattenberry E, et al.: Evaluation of SDHB, SDHD and VHL gene susceptibility testing in the assessment of individuals with non-syndromic phaeochromocytoma, paraganglioma and head and neck paraganglioma. Clin Endocrinol (Oxf) 78 (6): 898-906, 2013.
-
Pęczkowska M, Kowalska A, Sygut J, et al.: Testing new susceptibility genes in the cohort of apparently sporadic phaeochromocytoma/paraganglioma patients with clinical characteristics of hereditary syndromes. Clin Endocrinol (Oxf) 79 (6): 817-23, 2013.
-
Karasek D, Frysak Z, Pacak K: Genetic testing for pheochromocytoma. Curr Hypertens Rep 12 (6): 456-64, 2010.
-
Neumann HP, Bausch B, McWhinney SR, et al.: Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med 346 (19): 1459-66, 2002.
-
Fishbein L, Merrill S, Fraker DL, et al.: Inherited mutations in pheochromocytoma and paraganglioma: why all patients should be offered genetic testing. Ann Surg Oncol 20 (5): 1444-50, 2013.
-
Bacca A, Sellari Franceschini S, Carrara D, et al.: Sporadic or familial head neck paragangliomas enrolled in a single center: clinical presentation and genotype/phenotype correlations. Head Neck 35 (1): 23-7, 2013.
-
Rijken JA, Niemeijer ND, Corssmit EP, et al.: Low penetrance of paraganglioma and pheochromocytoma in an extended kindred with a germline SDHB exon 3 deletion. Clin Genet 89 (1): 128-32, 2016.
-
Lenders JW, Duh QY, Eisenhofer G, et al.: Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99 (6): 1915-42, 2014.
-
Hussain I, Husain Q, Baredes S, et al.: Molecular genetics of paragangliomas of the skull base and head and neck region: implications for medical and surgical management. J Neurosurg 120 (2): 321-30, 2014.
-
Comino-Méndez I, Gracia-Aznárez FJ, Schiavi F, et al.: Exome sequencing identifies MAX mutations as a cause of hereditary pheochromocytoma. Nat Genet 43 (7): 663-7, 2011.
-
Neumann HP, Sullivan M, Winter A, et al.: Germline mutations of the TMEM127 gene in patients with paraganglioma of head and neck and extraadrenal abdominal sites. J Clin Endocrinol Metab 96 (8): E1279-82, 2011.
-
Burnichon N, Lepoutre-Lussey C, Laffaire J, et al.: A novel TMEM127 mutation in a patient with familial bilateral pheochromocytoma. Eur J Endocrinol 164 (1): 141-5, 2011.
-
Bayley JP, Kunst HP, Cascon A, et al.: SDHAF2 mutations in familial and sporadic paraganglioma and phaeochromocytoma. Lancet Oncol 11 (4): 366-72, 2010.
-
Letouzé E, Martinelli C, Loriot C, et al.: SDH mutations establish a hypermethylator phenotype in paraganglioma. Cancer Cell 23 (6): 739-52, 2013.
-
van der Mey AG, Maaswinkel-Mooy PD, Cornelisse CJ, et al.: Genomic imprinting in hereditary glomus tumours: evidence for new genetic theory. Lancet 2 (8675): 1291-4, 1989.
-
Baysal BE: Mitochondrial complex II and genomic imprinting in inheritance of paraganglioma tumors. Biochim Biophys Acta 1827 (5): 573-7, 2013.
-
Amar L, Bertherat J, Baudin E, et al.: Genetic testing in pheochromocytoma or functional paraganglioma. J Clin Oncol 23 (34): 8812-8, 2005.
-
Neumann HP, Erlic Z, Boedeker CC, et al.: Clinical predictors for germline mutations in head and neck paraganglioma patients: cost reduction strategy in genetic diagnostic process as fall-out. Cancer Res 69 (8): 3650-6, 2009.
-
Rattenberry E, Vialard L, Yeung A, et al.: A comprehensive next generation sequencing-based genetic testing strategy to improve diagnosis of inherited pheochromocytoma and paraganglioma. J Clin Endocrinol Metab 98 (7): E1248-56, 2013.
-
Neumann HP, Pawlu C, Peczkowska M, et al.: Distinct clinical features of paraganglioma syndromes associated with SDHB and SDHD gene mutations. JAMA 292 (8): 943-51, 2004.
-
Ricketts CJ, Forman JR, Rattenberry E, et al.: Tumor risks and genotype-phenotype-proteotype analysis in 358 patients with germline mutations in SDHB and SDHD. Hum Mutat 31 (1): 41-51, 2010.
-
Welander J, Söderkvist P, Gimm O: Genetics and clinical characteristics of hereditary pheochromocytomas and paragangliomas. Endocr Relat Cancer 18 (6): R253-76, 2011.
-
Schiavi F, Milne RL, Anda E, et al.: Are we overestimating the penetrance of mutations in SDHB? Hum Mutat 31 (6): 761-2, 2010.
-
Solis DC, Burnichon N, Timmers HJ, et al.: Penetrance and clinical consequences of a gross SDHB deletion in a large family. Clin Genet 75 (4): 354-63, 2009.
-
Hes FJ, Weiss MM, Woortman SA, et al.: Low penetrance of a SDHB mutation in a large Dutch paraganglioma family. BMC Med Genet 11: 92, 2010.
-
Schiavi F, Boedeker CC, Bausch B, et al.: Predictors and prevalence of paraganglioma syndrome associated with mutations of the SDHC gene. JAMA 294 (16): 2057-63, 2005.
-
Peczkowska M, Cascon A, Prejbisz A, et al.: Extra-adrenal and adrenal pheochromocytomas associated with a germline SDHC mutation. Nat Clin Pract Endocrinol Metab 4 (2): 111-5, 2008.
-
Pasini B, McWhinney SR, Bei T, et al.: Clinical and molecular genetics of patients with the Carney-Stratakis syndrome and germline mutations of the genes coding for the succinate dehydrogenase subunits SDHB, SDHC, and SDHD. Eur J Hum Genet 16 (1): 79-88, 2008.
-
Horváth R, Abicht A, Holinski-Feder E, et al.: Leigh syndrome caused by mutations in the flavoprotein (Fp) subunit of succinate dehydrogenase (SDHA). J Neurol Neurosurg Psychiatry 77 (1): 74-6, 2006.
-
Burnichon N, Brière JJ, Libé R, et al.: SDHA is a tumor suppressor gene causing paraganglioma. Hum Mol Genet 19 (15): 3011-20, 2010.
-
Korpershoek E, Favier J, Gaal J, et al.: SDHA immunohistochemistry detects germline SDHA gene mutations in apparently sporadic paragangliomas and pheochromocytomas. J Clin Endocrinol Metab 96 (9): E1472-6, 2011.
-
Grandori C, Cowley SM, James LP, et al.: The Myc/Max/Mad network and the transcriptional control of cell behavior. Annu Rev Cell Dev Biol 16: 653-99, 2000.
-
Schiffman JD: No child left behind in SDHB testing for paragangliomas and pheochromocytomas. J Clin Oncol 29 (31): 4070-2, 2011.
-
Jasperson KW, Kohlmann W, Gammon A, et al.: Role of rapid sequence whole-body MRI screening in SDH-associated hereditary paraganglioma families. Fam Cancer 13 (2): 257-65, 2014.
-
Gravel G, Niccoli P, Rohmer V, et al.: The value of a rapid contrast-enhanced angio-MRI protocol in the detection of head and neck paragangliomas in SDHx mutations carriers: a retrospective study on behalf of the PGL.EVA investigators. Eur Radiol 26 (6): 1696-704, 2016.
-
Timmers HJ, Gimenez-Roqueplo AP, Mannelli M, et al.: Clinical aspects of SDHx-related pheochromocytoma and paraganglioma. Endocr Relat Cancer 16 (2): 391-400, 2009.
-
Lefebvre M, Foulkes WD: Pheochromocytoma and paraganglioma syndromes: genetics and management update. Curr Oncol 21 (1): e8-e17, 2014.
-
Pacak K: Preoperative management of the pheochromocytoma patient. J Clin Endocrinol Metab 92 (11): 4069-79, 2007.
-
GRAHAM JB: Pheochromocytoma and hypertension; an analysis of 207 cases. Int Abstr Surg 92 (2): 105-21, 1951.
-
Goldstein RE, O'Neill JA Jr, Holcomb GW 3rd, et al.: Clinical experience over 48 years with pheochromocytoma. Ann Surg 229 (6): 755-64; discussion 764-6, 1999.
-
Miura Y, Yoshinaga K: Doxazosin: a newly developed, selective alpha 1-inhibitor in the management of patients with pheochromocytoma. Am Heart J 116 (6 Pt 2): 1785-9, 1988.
-
Prys-Roberts C, Farndon JR: Efficacy and safety of doxazosin for perioperative management of patients with pheochromocytoma. World J Surg 26 (8): 1037-42, 2002.
-
Zhu Y, He HC, Su TW, et al.: Selective α1-adrenoceptor antagonist (controlled release tablets) in preoperative management of pheochromocytoma. Endocrine 38 (2): 254-9, 2010.
-
Ross EJ, Prichard BN, Kaufman L, et al.: Preoperative and operative management of patients with phaeochromocytoma. Br Med J 1 (5534): 191-8, 1967.
-
Hack HA: The perioperative management of children with phaeochromocytoma. Paediatr Anaesth 10 (5): 463-76, 2000.
-
Proye C, Thevenin D, Cecat P, et al.: Exclusive use of calcium channel blockers in preoperative and intraoperative control of pheochromocytomas: hemodynamics and free catecholamine assays in ten consecutive patients. Surgery 106 (6): 1149-54, 1989.
-
Vargas HI, Kavoussi LR, Bartlett DL, et al.: Laparoscopic adrenalectomy: a new standard of care. Urology 49 (5): 673-8, 1997.
-
Perrier ND, Kennamer DL, Bao R, et al.: Posterior retroperitoneoscopic adrenalectomy: preferred technique for removal of benign tumors and isolated metastases. Ann Surg 248 (4): 666-74, 2008.
-
Dickson PV, Jimenez C, Chisholm GB, et al.: Posterior retroperitoneoscopic adrenalectomy: a contemporary American experience. J Am Coll Surg 212 (4): 659-65; discussion 665-7, 2011.
-
Ober WB: Emil Zuckerkandl and his delightful little organ. Pathol Annu 18 Pt 1: 103-19, 1983.
-
Mundschenk J, Lehnert H: Malignant pheochromocytoma. Exp Clin Endocrinol Diabetes 106 (5): 373-6, 1998.
-
Grubbs EG, Rich TA, Ng C, et al.: Long-term outcomes of surgical treatment for hereditary pheochromocytoma. J Am Coll Surg 216 (2): 280-9, 2013.
-
Castinetti F, Qi XP, Walz MK, et al.: Outcomes of adrenal-sparing surgery or total adrenalectomy in phaeochromocytoma associated with multiple endocrine neoplasia type 2: an international retrospective population-based study. Lancet Oncol 15 (6): 648-55, 2014.
Carney-Stratakis SyndromeClinical Description Carney-Stratakis syndrome (CSS; also known as Carney-Stratakis dyad) was first described in 2002. Although similarly named, this syndrome is distinctly different from Carney Complex and Carney Triad (see Table 6). CSS is characterized by an autosomal dominant germline pathogenic variant in the succinate dehydrogenase (SDH) subunit B, C, or D (SDHx) genes that demonstrates incomplete penetrance. Affected individuals develop multifocal, locally aggressive gastrointestinal stromal tumors (GISTs) and multiple neck, intrathoracic, and intra-abdominal paragangliomas (PGLs) at relatively early ages.[1,2,3] CSS-associated GISTs and PGLs display phenotypes that differ from their sporadically occurring, more-common counterparts; as a result, it is important to understand the unique features of imaging, treatment, and surveillance in patients with CSS. Table 6. Comparison of Carney-Stratakis Syndrome, Carney Triad, and Carney Complex| Syndrome | Inheritance Pattern | Mean Age at Onset (y) | Affected Sex | Associated Lesions | Pathogenic Variants | Tumor Behavior |
|---|
| AD = autosomal dominant; GIST = gastrointestinal stromal tumor; F = female; M = male. | | Carney-Stratakis Syndrome[1,3,4] | AD | 23 | M, F | Paraganglioma, stomach epithelioid GIST | GermlineSDHxpathogenic variants; noKITorPDGFRApathogenic variants | GIST metastasis but protracted course; paraganglioma aggressive | | Carney Triad[4,5,6] | None | <30 | >95% F | Lung chondroma, paraganglioma, stomach epithelioid GIST | NoKIT,PDGFRA, orSDHxpathogenic variants | GIST metastasis but protracted course | | Carney Complex[7,8] | AD | 20 | M, F | Lentigines, myxomas, schwannoma, thyroid follicular adenomas or carcinoma, primary pigmented nodular adrenocortical disease, pituitary adenomas | GermlinePRKAR1Apathogenic variants | N/A | Genetics, Inheritance, and Genetic Testing The tumorigenesis of CSS-associated GISTs appears to involve succinate dehydrogenase deficiency rather than gain-of-function variants in the KIT or PDGFRA gene, as is seen in the vast majority of GISTs.[9] SDH deficiency is also a characteristic finding of pediatric-type GISTs; CSS-associated GISTs display clinical findings similar to these tumors, including young age at onset (median age, 19 years), specificity to the stomach, multifocality, and resistance to imatinib.[3,10,11,12] Furthermore, tumor size and mitotic rate do not accurately predict metastatic potential or survival, as SDH-deficient GISTs frequently metastasize to regional lymph nodes, the peritoneal cavity, and the liver; however, long-term survival is common.[6,13] Refer to the Genetics, Inheritance, and Genetic Testing section in the Familial PGL section of this summary for more information about genetic testing for the genes involved in CSS. Surveillance Although the natural history of CSS is poorly understood, experts recommend that ongoing surveillance include the following: close patient follow-up with annual history that focuses on symptoms of anemia and catecholamine excess, physical exam, biochemical analysis with plasma metanephrine level and chromogranin A to detect recurrent PGLs, and cross-sectional imaging. Although many PGLs do not secrete catecholamines, chromogranin A has been found to be elevated in PGLs and may be a useful marker for tumor recurrence. The appropriate screening imaging modality is unknown at this time, but fluorine F 18-fluorodeoxyglucose positron emission tomography-computed tomography (18F-FDG PET-CT) is highly sensitive at identifying extra-adrenal PGLs and GISTs. Because of the risks of ionizing radiation exposure from CT, some suggest using MRI for annual surveillance.[14,15] Level of evidence: 4 Interventions Because multiple primary GISTs and PGLs are common with CSS, preoperative imaging is paramount to accurately identify the extent of disease before surgical planning. Most patients will present having already undergone imaging with CT or magnetic resonance imaging (MRI). Both methods have excellent sensitivity for identifying PGLs, but additional functional imaging is recommended because of the diffuse nature of these tumors. 18F-FDG PET-CT is superior to iodine I 123-metaiodobenzylguanidine at identifying SDHx-associated PGLs and, because of the high metabolic activity of GISTs, has excellent sensitivity in identifying them.[14,16] Thus, in patients with SDHx pathogenic variants, including those with CSS, 18F-FDG PET-CT is the preferred functional imaging modality to optimally detect and stage all GISTs and PGLs.[15] Some evidence suggests that 18F-fluoro-L-dihydroxyphenylalanine (18F-FDOPA) PET-CT is superior at identifying the primary PGL, while 18F-FDG PET-CT is superior at identifying metastases. There are no prospective treatment studies involving patients with CSS; therefore, recommendations are based on limited clinical experience, single case series, and extrapolations from genetically-similar tumors with similar clinical behavior. The mainstay of treatment for CSS-associated GISTs and PGLs is complete surgical resection of the tumor. The timing of the operation correlates with the presentation of the tumor. Surgical resection can be accomplished with laparoscopic or open techniques. For PGLs, vascular reconstruction is uncommon. Although PGLs are commonly present in the paraaortic region, the need for major vascular reconstruction is uncommon. GIST tumors can be resected with wedge resection and primary closure and re-anastomosis. Ensuring negative margins is important, as patients for whom a complete resection is accomplished experience the longest survival.[17] In the rare setting of synchronous disease, combined resection is appropriate if tolerable by the patient. More commonly, tumors develop metachronously, with GISTs arising first; individual resection occurs at the time of diagnosis of each tumor. A thorough preoperative endoscopy and complete surgical exploration of the stomach are essential, as multiple separate GISTs are frequently encountered. The high frequency of multifocality and the likelihood of tumor recurrence do not justify a prophylactic total gastrectomy because of its substantial associated morbidity. Furthermore, a total gastrectomy is generally only performed when the current disease burden precludes a lesser resection. To this end, gastric wedge resection with gross negative margins is the surgical goal.[18] Sampling of any suspicious nodes at the time of resection is commonly performed. Evidence suggests that locally advanced CSS-associated GISTs demonstrate a rather indolent course;[19] thus, the concern for nodal involvement based on preoperative imaging or abdominal exploration need not deter resection of the primary tumor. While a role for neoadjuvant imatinib in locally advanced adult-type GISTs has been widely described to improve resectability or reduce the burden of resection, it is unlikely to have any effect in locally advanced SDH-deficient GISTs.[20] Evidence suggests that for these tumors, the second-line targeted agents, including sorafenib, sunitinib, dasatinib, and nilotinib, may be beneficial in the adjuvant setting.[21,22] No data support using these agents in the neoadjuvant setting at this time. Regarding treatment of CSS-associated PGLs, patients are commonly initiated on alpha-blockade preoperatively to minimize perioperative cardiac morbidity and mortality. PGLs typically occur in the para-aortic chain from the urinary bladder and the aortic bifurcation to the superior mediastinum and head and neck. As in the treatment of GISTs, the operative goal is resection of all known disease. Preoperative imaging and intra-operative exploration are essential to achieving this goal. Multiple tumors are common; when disease is present in the bilateral adrenal glands, the surgeon faces the possibility of rendering a patient steroid dependent with a lifelong risk of a fatal Addisonian crisis. In this setting, a surgeon proficient in performing a cortical-sparing adrenalectomy may be consulted. Level of evidence: 5 References:
-
Carney JA, Stratakis CA: Familial paraganglioma and gastric stromal sarcoma: a new syndrome distinct from the Carney triad. Am J Med Genet 108 (2): 132-9, 2002.
-
McWhinney SR, Pasini B, Stratakis CA, et al.: Familial gastrointestinal stromal tumors and germ-line mutations. N Engl J Med 357 (10): 1054-6, 2007.
-
Pasini B, McWhinney SR, Bei T, et al.: Clinical and molecular genetics of patients with the Carney-Stratakis syndrome and germline mutations of the genes coding for the succinate dehydrogenase subunits SDHB, SDHC, and SDHD. Eur J Hum Genet 16 (1): 79-88, 2008.
-
Gaal J, Stratakis CA, Carney JA, et al.: SDHB immunohistochemistry: a useful tool in the diagnosis of Carney-Stratakis and Carney triad gastrointestinal stromal tumors. Mod Pathol 24 (1): 147-51, 2011.
-
Agaimy A, Pelz AF, Corless CL, et al.: Epithelioid gastric stromal tumours of the antrum in young females with the Carney triad: a report of three new cases with mutational analysis and comparative genomic hybridization. Oncol Rep 18 (1): 9-15, 2007.
-
Zhang L, Smyrk TC, Young WF Jr, et al.: Gastric stromal tumors in Carney triad are different clinically, pathologically, and behaviorally from sporadic gastric gastrointestinal stromal tumors: findings in 104 cases. Am J Surg Pathol 34 (1): 53-64, 2010.
-
Boikos SA, Stratakis CA: Carney complex: pathology and molecular genetics. Neuroendocrinology 83 (3-4): 189-99, 2006.
-
Correa R, Salpea P, Stratakis CA: Carney complex: an update. Eur J Endocrinol 173 (4): M85-97, 2015.
-
Hensen EF, Bayley JP: Recent advances in the genetics of SDH-related paraganglioma and pheochromocytoma. Fam Cancer 10 (2): 355-63, 2011.
-
Agaram NP, Laquaglia MP, Ustun B, et al.: Molecular characterization of pediatric gastrointestinal stromal tumors. Clin Cancer Res 14 (10): 3204-15, 2008.
-
Miettinen M, Wang ZF, Sarlomo-Rikala M, et al.: Succinate dehydrogenase-deficient GISTs: a clinicopathologic, immunohistochemical, and molecular genetic study of 66 gastric GISTs with predilection to young age. Am J Surg Pathol 35 (11): 1712-21, 2011.
-
Sawhney SA, Chapman AD, Carney JA, et al.: Incomplete Carney triad--a review of two cases. QJM 102 (9): 649-53, 2009.
-
Rege TA, Wagner AJ, Corless CL, et al.: "Pediatric-type" gastrointestinal stromal tumors in adults: distinctive histology predicts genotype and clinical behavior. Am J Surg Pathol 35 (4): 495-504, 2011.
-
Ayala-Ramirez M, Callender GG, Kupferman ME, et al.: Paraganglioma syndrome type 1 in a patient with Carney-Stratakis syndrome. Nat Rev Endocrinol 6 (2): 110-5, 2010.
-
Timmers HJ, Kozupa A, Chen CC, et al.: Superiority of fluorodeoxyglucose positron emission tomography to other functional imaging techniques in the evaluation of metastatic SDHB-associated pheochromocytoma and paraganglioma. J Clin Oncol 25 (16): 2262-9, 2007.
-
Timmers HJ, Chen CC, Carrasquillo JA, et al.: Comparison of 18F-fluoro-L-DOPA, 18F-fluoro-deoxyglucose, and 18F-fluorodopamine PET and 123I-MIBG scintigraphy in the localization of pheochromocytoma and paraganglioma. J Clin Endocrinol Metab 94 (12): 4757-67, 2009.
-
Abadin SS, Ayala-Ramirez M, Jimenez C, et al.: Impact of surgical resection for subdiaphragmatic paragangliomas. World J Surg 38 (3): 733-41, 2014.
-
Demetri GD, Benjamin RS, Blanke CD, et al.: NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST)--update of the NCCN clinical practice guidelines. J Natl Compr Canc Netw 5 (Suppl 2): S1-29; quiz S30, 2007.
-
Maki RG, Blay JY, Demetri GD, et al.: Key Issues in the Clinical Management of Gastrointestinal Stromal Tumors: An Expert Discussion. Oncologist 20 (7): 823-30, 2015.
-
Ganjoo KN, Villalobos VM, Kamaya A, et al.: A multicenter phase II study of pazopanib in patients with advanced gastrointestinal stromal tumors (GIST) following failure of at least imatinib and sunitinib. Ann Oncol 25 (1): 236-40, 2014.
-
Gill AJ, Chou A, Vilain R, et al.: Immunohistochemistry for SDHB divides gastrointestinal stromal tumors (GISTs) into 2 distinct types. Am J Surg Pathol 34 (5): 636-44, 2010.
-
Janeway KA, Albritton KH, Van Den Abbeele AD, et al.: Sunitinib treatment in pediatric patients with advanced GIST following failure of imatinib. Pediatr Blood Cancer 52 (7): 767-71, 2009.
Changes to This Summary (04 / 14 / 2017)The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above. Multiple Endocrine Neoplasia Type 2 This section was extensively revised. This summary is written and maintained by the PDQ Cancer Genetics Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® - NCI's Comprehensive Cancer Database pages. About This PDQ SummaryPurpose of This Summary This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the genetics of endocrine and neuroendocrine neoplasias. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions. Reviewers and Updates This summary is reviewed regularly and updated as necessary by the PDQ Cancer Genetics Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH). Board members review recently published articles each month to determine whether an article should: - be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary. The lead reviewers for Genetics of Endocrine and Neuroendocrine Neoplasias are: - Kathleen A. Calzone, PhD, RN, AGN-BC, FAAN (National Cancer Institute)
- Sarah Nielsen, MS, LCGC (The University of Chicago)
- Suzanne M. O'Neill, MS, PhD, CGC (Northwestern University)
- Nancy D. Perrier, MD, FACS (University of Texas, M.D. Anderson Cancer Center)
- Beth N. Peshkin, MS, CGC (Lombardi Comprehensive Cancer Center at Georgetown University Medical Center)
- Susan K. Peterson, PhD, MPH (University of Texas, M.D. Anderson Cancer Center)
- Jennifer Sipos, MD (The Ohio State University)
- Deborah E. Tamura, MS, RN, APNG (National Cancer Institute)
- Susan T. Vadaparampil, PhD, MPH (H. Lee Moffitt Cancer Center & Research Institute)
- Catharine Wang, PhD, MSc (Boston University School of Public Health)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries. Levels of Evidence Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Cancer Genetics Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations. Permission to Use This Summary PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary]." The preferred citation for this PDQ summary is: PDQ® Cancer Genetics Editorial Board. PDQ Genetics of Endocrine and Neuroendocrine Neoplasias. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/thyroid/hp/medullary-thyroid-genetics-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389271] Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images. Disclaimer The information in these summaries should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page. Contact Us More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's Email Us. Last Revised: 2017-04-14 Last modified on: 8 September 2017
|
|