General Information About Childhood Acute Myeloid Leukemia and Other Myeloid Malignancies
Childhood acute myeloid leukemia (AML) is a type of cancer in which the bone marrow makes a large number of abnormal blood cells.
Childhood acute myeloid leukemia (AML) is a cancer of the blood and bone marrow. AML is also called acute myelogenous leukemia, acute myeloblastic leukemia, acute granulocytic leukemia, and acute nonlymphocytic leukemia. Cancers that are acute usually get worse quickly if they are not treated. Cancers that are chronic usually get worse slowly.
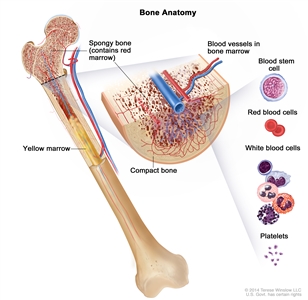
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
Leukemia and other diseases of the blood and bone marrow may affect red blood cells, white blood cells, and platelets.
Normally, the bone marrow makes blood stem cells (immature cells) that become mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell. A lymphoid stem cell becomes a white blood cell.
A myeloid stem cell becomes one of three types of mature blood cells:
- Red blood cells that carry oxygen and other substances to all tissues of the body.
- White blood cells that fight infection and disease.
- Platelets that form blood clots to stop bleeding.
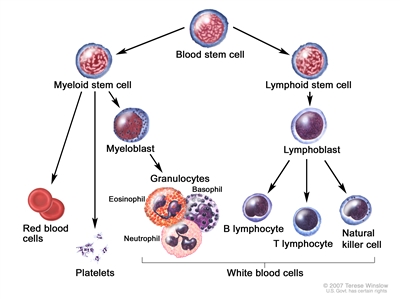
Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell.
In AML, the myeloid stem cells usually become a type of immature white blood cell called myeloblasts (or myeloid blasts). The myeloblasts, or leukemia cells, in AML are abnormal and do not become healthy white blood cells. The leukemia cells can build up in the blood and bone marrow so there is less room for healthy white blood cells, red blood cells, and platelets. When this happens, infection, anemia, or easy bleeding may occur. The leukemia cells can spread outside the blood to other parts of the body, including the central nervous system (brain and spinal cord), skin, and gums. Sometimes leukemia cells form a solid tumor called a granulocytic sarcoma or chloroma.
There are subtypes of AML based on the type of blood cell that is affected. The treatment of AML is different when it is a subtype called acute promyelocytic leukemia (APL) or when the child has Down syndrome.
Other myeloid diseases can affect the blood and bone marrow.
Chronic myelogenous leukemia
In chronic myelogenous leukemia (CML), too many bone marrow stem cells become a type of white blood cell called granulocytes. Some of these bone marrow stem cells never become mature white blood cells. These are called blasts. Over time, the granulocytes and blasts crowd out the red blood cells and platelets in the bone marrow. CML is rare in children.
Juvenile myelomonocytic leukemia
Juvenile myelomonocytic leukemia (JMML) is a rare childhood cancer that occurs more often in children around the age of 2 years and is more common in boys. In JMML, too many bone marrow stem cells become 2 types of white blood cells called myelocytes and monocytes. Some of these bone marrow stem cells never become mature white blood cells. These immature cells, called blasts, are unable to do their usual work. Over time, the myelocytes, monocytes, and blasts crowd out the red blood cells and platelets in the bone marrow. When this happens, infection, anemia, or easy bleeding may occur.
Myelodysplastic syndromes
Myelodysplastic syndromes (MDS) occur less often in children than in adults. In MDS, the bone marrow makes too few red blood cells, white blood cells, and platelets. These blood cells may not mature and enter the blood. The treatment for MDS depends on how low the numbers of red blood cells, white blood cells, or platelets are. Over time, MDS may become AML.
Transient myeloproliferative disorder (TMD) is a type of MDS. This disorder of the bone marrow can develop in newborns who have Down syndrome. It usually goes away on its own within the first 3 weeks of life. Infants who have Down syndrome and TMD have an increased chance of developing AML before the age of 3 years.
This summary is about childhood AML, childhood CML, JMML, and MDS. See the following PDQ summaries for more information about other types of leukemia and diseases of the blood and bone marrow in children and adults:
- Childhood Acute Lymphoblastic Leukemia Treatment
- Adult Acute Myeloid Leukemia Treatment
- Adult Acute Lymphoblastic Leukemia Treatment
- Chronic Myelogenous Leukemia Treatment
- Chronic Lymphocytic Leukemia Treatment
- Hairy Cell Leukemia Treatment
- Myelodysplastic Syndromes Treatment
- Myelodysplastic/Myeloproliferative Neoplasms Treatment
AML or MDS may occur after treatment with certain anticancer drugs and/or radiation therapy.
Cancer treatment with certain anticancer drugs and/or radiation therapy may cause therapy -related AML (t-AML) or therapy-related MDS (t-MDS). The risk of these therapy-related myeloid diseases depends on the total dose of the anticancer drugs used and the radiation dose and treatment field. Some patients also have an inherited risk for t-AML and t-MDS. These therapy-related diseases usually occur within 7 years after treatment, but are rare in children.
The risk factors for childhood AML, childhood CML, JMML, and MDS are similar.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn't mean that you will not get cancer. Talk with your child's doctor if you think your child may be at risk. These and other factors may increase the risk of childhood AML, childhood CML, JMML, and MDS:
- Having a brother or sister, especially a twin, with leukemia.
- Being Hispanic.
- Being exposed to cigarette smoke or alcohol before birth.
- Having a personal history of aplastic anemia.
- Having a personal or family history of MDS.
- Having a family history of AML.
- Past treatment with chemotherapy or radiation therapy.
- Being exposed to ionizing radiation or chemicals such as benzene.
- Having certain genetic disorders, such as:
- Down syndrome.
- Fanconi anemia.
- Neurofibromatosis type 1.
- Noonan syndrome.
- Shwachman-Diamond syndrome.
Signs and symptoms of childhood AML, childhood CML, JMML, or MDS include fever, feeling tired, and easy bleeding or bruising.
These and other signs and symptoms may be caused by childhood AML, childhood CML, JMML, or MDS or by other conditions. Check with a doctor if your child has any of the following:
- Fever with or without an infection.
- Night sweats.
- Shortness of breath.
- Weakness or feeling tired.
- Easy bruising or bleeding.
- Petechiae (flat, pinpoint spots under the skin caused by bleeding).
- Pain in the bones or joints.
- Pain or feeling of fullness below the ribs.
- Painless lumps in the neck, underarm, stomach, groin, or other parts of the body. In childhood AML, these lumps, called leukemia cutis, may be blue or purple.
- Painless lumps that are sometimes around the eyes. These lumps, called chloromas, are sometimes seen in childhood AML and may be blue-green.
- An eczema -like skin rash.
The signs and symptoms of TMD may include the following:
- Swelling all over the body.
- Shortness of breath.
- Trouble breathing.
- Weakness or feeling tired.
- Pain below the ribs.
Tests that examine the blood and bone marrow are used to detect (find) and diagnose childhood AML, childhood CML, JMML, and MDS.
The following tests and procedures may be used:
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options for childhood AML depend on the following:
- The age of the child when the cancer is diagnosed.
- The race or ethnic group of the child.
- Whether the child is greatly overweight.
- Number of white blood cells in the blood at diagnosis.
- Whether the AML occurred after previous cancer treatment.
- The subtype of AML.
- Whether there are certain chromosome or gene changes in the leukemia cells.
- Whether the child has Down syndrome. Most children with AML and Down syndrome can be cured of their leukemia.
- Whether the leukemia is in the central nervous system (brain and spinal cord).
- How quickly the leukemia responds to treatment.
- Whether the AML is newly diagnosed (untreated) or has recurred (come back) after being treated.
- The length of time since treatment ended, for AML that has recurred.
The prognosis and treatment options for childhood CML depend on how long it has been since the patient was diagnosed and how many blast cells are in the blood.
The prognosis (chance of recovery) and treatment options for JMML depend on the following:
- The age of the child when the cancer is diagnosed.
- The type of gene affected and the number of genes that have changes.
- How many red blood cells, white blood cells, or platelets are in the blood.
- Whether the JMML is newly diagnosed (untreated) or has recurred after treatment.
The prognosis (chance of recovery) and treatment options for MDS depend on the following:
- Whether the MDS was caused by previous cancer treatment.
- How low the numbers of red blood cells, white blood cells, or platelets are.
- Whether the MDS is newly diagnosed (untreated) or has recurred after treatment.
Stages of Childhood Acute Myeloid Leukemia and Other Myeloid Malignancies
Once childhood acute myeloid leukemia (AML) has been diagnosed, tests are done to find out if the cancer has spread to other parts of the body.
The following tests and procedures may be used to determine if the leukemia has spread:
- Lumbar puncture: A procedure used to collect a sample of cerebrospinal fluid (CSF) from the spinal column. This is done by placing a needle between two bones in the spine and into the CSF around the spinal cord and removing a sample of the fluid. The sample of CSF is checked under a microscope for signs that leukemia cells have spread to the brain and spinal cord. This procedure is also called an LP or spinal tap.
- Biopsy of the testicles, ovaries, or skin: The removal of cells or tissues from the testicles, ovaries, or skin so they can be viewed under a microscope to check for signs of cancer. This is done only if something unusual about the testicles, ovaries, or skin is found during the physical exam.
There is no standard staging system for childhood AML, childhood chronic myelogenous leukemia (CML), juvenile myelomonocytic leukemia (JMML), or myelodysplastic syndromes (MDS).
The extent or spread of cancer is usually described as stages. Instead of stages, treatment of childhood AML, childhood CML, JMML, and MDS is based on one or more of the following:
- The type of disease or the subtype of AML.
- Whether leukemia has spread outside the blood and bone marrow.
- Whether the disease is newly diagnosed, in remission, or recurrent.
Newly diagnosed childhood AML
Newly diagnosed childhood AML has not been treated except to relieve signs and symptoms such as fever, bleeding, or pain, and one of the following is true:
- More than 20% of the cells in the bone marrow are blasts (leukemia cells).
or
- Less than 20% of the cells in the bone marrow are blasts and there is a specific change in the chromosome.
Childhood AML in remission
In childhood AML in remission, the disease has been treated and the following are true:
- The complete blood count is almost normal.
- Less than 5% of the cells in the bone marrow are blasts (leukemia cells).
- There are no signs or symptoms of leukemia in the brain, spinal cord, or other parts of the body.
Recurrent Childhood Acute Myeloid Leukemia
Recurrent childhood acute myeloid leukemia (AML) has recurred (come back) after it has been treated. The cancer may come back in the blood and bone marrow or in other parts of the body, such as the central nervous system (brain and spinal cord).
Treatment Option Overview
There are different types of treatment for children with acute myeloid leukemia (AML), chronic myelogenous leukemia (CML), juvenile myelomonocytic leukemia (JMML), or myelodysplastic syndromes (MDS).
Different types of treatment are available for children with AML, CML, JMML, or MDS. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment.
Because cancer in children is rare, taking part in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment.
Treatment is planned by a team of health care providers who are experts in treating childhood leukemia and other diseases of the blood.
Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other healthcare providers who are experts in treating children with leukemia and who specialize in certain areas of medicine. These may include the following specialists:
- Pediatrician.
- Hematologist.
- Medical oncologist.
- Pediatric surgeon.
- Radiation oncologist.
- Neurologist.
- Neuropathologist.
- Neuroradiologist.
- Pediatric nurse specialist.
- Social worker.
- Rehabilitation specialist.
- Psychologist.
Some cancer treatments cause side effects months or years after treatment has ended.
Regular follow-up exams are very important. Some cancer treatments cause side effects that continue or appear months or years after cancer treatment has ended. These are called late effects. Late effects of cancer treatment may include:
- Physical problems.
- Changes in mood, feelings, thinking, learning, or memory.
- Second cancers (new types of cancer).
Some late effects may be treated or controlled. It is important that parents of children who are treated for AML or other blood diseases talk with their doctors about the effects cancer treatment can have on their child. (See the PDQ summary on Late Effects of Treatment for Childhood Cancer for more information).
The treatment of childhood AML usually has two phases.
The treatment of childhood AML is done in phases:
- Induction therapy: This is the first phase of treatment. The goal is to kill the leukemia cells in the blood and bone marrow. This puts the leukemia into remission.
- Consolidation /intensification therapy: This is the second phase of treatment. It begins once the leukemia is in remission. The goal of therapy is to kill any remaining leukemia cells that may not be active but could begin to regrow and cause a relapse.
Treatment called central nervous system (CNS) sanctuary therapy may be given during the induction phase of therapy. Because standard doses of chemotherapy may not reach leukemia cells in the CNS (brain and spinal cord), the cells are able to find sanctuary (hide) in the CNS. Intrathecal chemotherapy is able to reach leukemia cells in the CNS. It is given to kill the leukemia cells and lessen the chance the leukemia will recur (come back). CNS sanctuary therapy is also called CNS prophylaxis.
Seven types of standard treatment are used for childhood AML, childhood CML, JMML, or MDS.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid (intrathecal chemotherapy), an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). Combination chemotherapy is treatment using more than one anticancer drug.
The way the chemotherapy is given depends on the type of cancer being treated.
In AML, the leukemia cells may spread to the brain and/or spinal cord. Chemotherapy given by mouth or vein to treat AML may not cross the blood-brain barrier to get into the fluid that surrounds the brain and spinal cord. Instead, chemotherapy is injected into the fluid-filled space to kill leukemia cells that may have spread there (intrathecal chemotherapy).
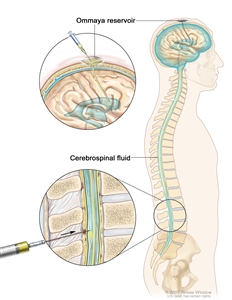
Intrathecal chemotherapy. Anticancer drugs are injected into the intrathecal space, which is the space that holds the cerebrospinal fluid (CSF, shown in blue). There are two different ways to do this. One way, shown in the top part of the figure, is to inject the drugs into an Ommaya reservoir (a dome-shaped container that is placed under the scalp during surgery; it holds the drugs as they flow through a small tube into the brain). The other way, shown in the bottom part of the figure, is to inject the drugs directly into the CSF in the lower part of the spinal column, after a small area on the lower back is numbed.
See Drugs Approved for Acute Myeloid Leukemia for more information.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type of the cancer being treated. In childhood AML, external radiation therapy may be used to treat a chloroma that does not respond to chemotherapy.
Stem cell transplant
Stem cell transplant is a way of giving chemotherapy and replacing blood-forming cells that are abnormal or destroyed by the cancer treatment. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the chemotherapy is completed, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body's blood cells.
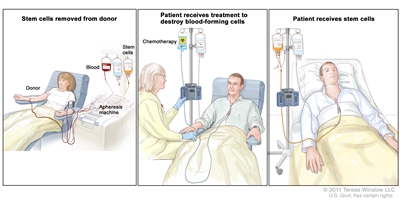
Stem cell transplant. (Step 1): Blood is taken from a vein in the arm of the donor. The patient or another person may be the donor. The blood flows through a machine that removes the stem cells. Then the blood is returned to the donor through a vein in the other arm. (Step 2): The patient receives chemotherapy to kill blood-forming cells. The patient may receive radiation therapy (not shown). (Step 3): The patient receives stem cells through a catheter placed into a blood vessel in the chest.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Types of targeted therapy include the following:
- Tyrosine kinase inhibitor therapy: Tyrosine kinase inhibitor (TKI) therapy blocks signals needed for tumors to grow. TKIs block the enzyme (tyrosine kinase) that causes stem cells to become more white blood cells (granulocytes or blasts) than the body needs. TKIs may be used with other anticancer drugs as adjuvant therapy (treatment given after the initial treatment, to lower the risk that the cancer will come back).
- Imatinib is a type of TKI that is approved to treat childhood CML.
- Sorafenib, dasatinib, and nilotinib are being studied in the treatment of childhood leukemia.
- Monoclonal antibody therapy: Monoclonal antibody therapy uses antibodies made in the laboratory, from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells.
- Gemtuzumab is a type of monoclonal antibody used in the treatment of a subtype of AML called acute promyelocytic leukemia (APL). Gemtuzumab is not available in the United States unless special approval is given. Monoclonal antibodies may be used with chemotherapy as adjuvant therapy.
- Proteasome inhibitor therapy: Proteasome inhibitors break down proteins in cancer cells and kill them.
- Bortezomib is a proteasome inhibitor used to treat childhood APL.
See Drugs Approved for Leukemia for more information.
Other drug therapy
Lenalidomide may be used to lessen the need for transfusions in patients who have myelodysplastic syndromes caused by a specific chromosome change.
Arsenic trioxide and all-trans retinoic acid (ATRA) are anticancer drugs that kill leukemia cells, stop the leukemia cells from dividing, or help the leukemia cells mature into white blood cells. These drugs are used in the treatment of acute promyelocytic leukemia.
See Drugs Approved for Acute Myeloid Leukemia for more information.
Watchful waiting
Watchful waiting is closely monitoring a patient's condition without giving any treatment until signs or symptoms appear or change. It is sometimes used to treat MDS or TMD.
Supportive care
Supportive care is given to lessen the problems caused by the disease or its treatment. Supportive care may include the following:
- Transfusion therapy: A way of giving red blood cells, white blood cells, or platelets to replace blood cells destroyed by disease or cancer treatment. The blood may be donated from another person or it may have been taken from the patient earlier and stored until needed.
- Drug therapy, such as antibiotics or antifungal agents.
- Leukapheresis: A procedure in which a special machine is used to remove white blood cells from the blood. Blood is taken from the patient and put through a blood cell separator where the white blood cells are removed. The rest of the blood is then returned to the patient's bloodstream.
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI website.
Biologic therapy
Biologic therapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer. This type of cancer treatment is also called biotherapy or immunotherapy.
Natural killer (NK) cells are a type of biologic therapy. NK cells are white blood cells that can kill tumor cells. These may be taken from a donor and given to the patient by infusion to help kill leukemia cells.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. See the Treatment Options section that follows for links to current treatment clinical trials. These have been retrieved from NCI's listing of clinical trials.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment Options for Childhood Acute Myeloid Leukemia, Childhood Chronic Myelogenous Leukemia, Juvenile Myelomonocytic Leukemia, and Myelodysplastic Syndromes
Newly Diagnosed Childhood Acute Myeloid Leukemia
Treatment of newly diagnosed childhood acute myeloid leukemia may include the following:
- Combination chemotherapy plus central nervous system sanctuary therapy with intrathecal chemotherapy.
- A clinical trial comparing different chemotherapy regimens (doses and schedules of treatment).
- A clinical trial of combination chemotherapy and targeted therapy with a proteasome inhibitor or a tyrosine kinase inhibitor with or without stem cell transplant.
Treatment of newly diagnosed childhood acute leukemia with a granulocytic sarcoma (chloroma) may include chemotherapy with or without radiation therapy.
Treatment of therapy -related AML is usually the same as for newly diagnosed AML, followed by stem cell transplant.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with untreated childhood acute myeloid leukemia and other myeloid malignancies. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your child's doctor about clinical trials that may be right for your child. General information about clinical trials is available from the NCI website.
Children with Newly Diagnosed Childhood AML and Down Syndrome
Treatment of acute myeloid leukemia (AML) in children aged 4 years or younger who have Down syndrome may include the following:
- Combination chemotherapy plus central nervous system sanctuary therapy with intrathecal chemotherapy.
Treatment of AML in children older than 4 years who have Down syndrome may be the same as treatment for children without Down syndrome.
Childhood Acute Myeloid Leukemia in Remission
Treatment of childhood acute myeloid leukemia (AML) during the remission phase (consolidation /intensification therapy) depends on the subtype of AML and may include the following:
- Combination chemotherapy.
- High-dose chemotherapy followed by stem cell transplant using blood stem cells from a donor.
- A clinical trial of chemotherapy followed by an infusion of natural killer cells.
- A clinical trial of combination chemotherapy and targeted therapy with a proteasome inhibitor or a tyrosine kinase inhibitor with or without stem cell transplant.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with childhood acute myeloid leukemia in remission. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your child's doctor about clinical trials that may be right for your child. General information about clinical trials is available from the NCI website.
Recurrent Childhood Acute Myeloid Leukemia
Treatment of recurrent childhood acute myeloid leukemia (AML) may include the following:
- Combination chemotherapy.
- Combination chemotherapy and stem cell transplant.
- A second stem cell transplant.
- A clinical trial of combinations of new anticancer drugs, new biologic agents, and stem cell transplant using different sources of stem cells.
Treatment of recurrent AML in children with Down syndrome is chemotherapy. It is not clear if stem cell transplant after chemotherapy is helpful in treating these children.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with recurrent childhood acute myeloid leukemia. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your child's doctor about clinical trials that may be right for your child. General information about clinical trials is available from the NCI website.
Acute Promyelocytic Leukemia
Treatment of acute promyelocytic leukemia may include the following:
- All-trans retinoic acid (ATRA) plus chemotherapy.
- Arsenic trioxide therapy.
- Central nervous system sanctuary therapy with intrathecal chemotherapy.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with childhood acute promyelocytic leukemia (M3). For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your child's doctor about clinical trials that may be right for your child. General information about clinical trials is available from the NCI website.
Recurrent Acute Promyelocytic Leukemia
Treatment of recurrent acute promyelocytic leukemia may include the following:
- All-trans retinoic acid therapy (ATRA) plus chemotherapy.
- Arsenic trioxide therapy.
- Targeted therapy with a monoclonal antibody (gemtuzumab), if special approval is given.
- Stem cell transplant using blood stem cells from the patient or a donor.
Childhood Chronic Myelogenous Leukemia
Treatment for childhood chronic myelogenous leukemia may include the following:
- Targeted therapy with a tyrosine kinase inhibitor (imatinib).
- A clinical trial of targeted therapy with other tyrosine kinase inhibitors.
For patients whose disease does not respond to therapy with imatinib or whose disease comes back after treatment, treatment may include the following:
- Stem cell transplant using blood stem cells from a donor.
- A clinical trial of targeted therapy with other tyrosine kinase inhibitors.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with childhood chronic myelogenous leukemia. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your child's doctor about clinical trials that may be right for your child. General information about clinical trials is available from the NCI website.
Juvenile Myelomonocytic Leukemia
Treatment of juvenile myelomonocytic leukemia (JMML) may include the following:
- Combination chemotherapy followed by stem cell transplant. If JMML recurs after stem cell transplant, a second stem cell transplant may be done.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with juvenile myelomonocytic leukemia. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your child's doctor about clinical trials that may be right for your child. General information about clinical trials is available from the NCI website.
Myelodysplastic Syndromes
Treatment of myelodysplastic syndromes (MDS) may include the following:
- Watchful waiting.
- Stem cell transplant using blood stem cells from a donor.
- Combination chemotherapy.
- Lenalidomide therapy.
- A clinical trial of stem cell transplant using lower doses of chemotherapy.
- A clinical trial of a new anticancer drug or targeted therapy.
If the MDS becomes acute myeloid leukemia (AML), treatment will be the same as treatment for newly diagnosed AML.
Treatment of therapy-related MDS is usually the same as for newly diagnosed AML, followed by stem cell transplant.
Transient myeloproliferative disorder (TMD), a type of MDS, usually goes away on its own. For TMD that does not go away on its own, treatment may include the following:
- Transfusion therapy.
- Leukapheresis.
- Chemotherapy.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with childhood myelodysplastic syndromes. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your child's doctor about clinical trials that may be right for your child. General information about clinical trials is available from the NCI website.
To Learn More About Childhood Acute Myeloid Leukemia and Other Myeloid Malignancies
For more information from the National Cancer Institute about childhood acute myeloid leukemia and other myeloid malignancies, see the following:
- What You Need to Know About™ Leukemia
- Drugs Approved for Acute Myeloid Leukemia
- Drugs Approved for Myeloproliferative Neoplasms
- Blood-Forming Stem Cell Transplants
- Targeted Cancer Therapies
For more childhood cancer information and other general cancer resources, see the following:
- About Cancer
- Childhood Cancers
- CureSearch for Children's Cancer
- Late Effects of Treatment for Childhood Cancer
- Adolescents and Young Adults with Cancer
- Children with Cancer: A Guide for Parents
- Cancer in Children and Adolescents
- Staging
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors and Caregivers
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood acute myeloid leukemia and other myeloid malignancies. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials are listed in PDQ and can be found online at NCI's website. Many cancer doctors who take part in clinical trials are also listed in PDQ. For more information, call the Cancer Information Service 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Acute Myeloid Leukemia/Other Myeloid Malignancies Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/leukemia/patient/child-aml-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389303]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 2,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2017-03-06
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.